I Have the Breast Cancer Gene. Finding the Positives in the BRCA-1 Mutation.
Receiving the results of my genetic testing was a confronting experience. In this post I talk about how I had fought to get my genes tested in the midst of chemo in order to make an informed decision regarding surgery. I also highlight the positives of being a breast cancer patient with the BRCA-1 mutation such as better prognosis and more treatment options.
In a small cramped office, my fiance and I were seated to hear the results of my genetic testing. I had invited my parents along but I wasn’t nervous at all, because I knew in my heart I wouldn’t test positive.
How could I possibly have the breast cancer genes when I had no family history of breast cancer?
But maybe I should have braced myself for the worst. That way I wouldn’t have been so shocked, and hurt by the results.
It felt like someone had punched me in the guts.
When the genetics councillor told me that I had tested positive for the BRCA-1 mutation, I couldn’t stop crying.
Even though I was only 29 when I was diagnosed - so uncharacteristically young for someone with breast cancer- not one of my doctors brought up the subject of genetic testing.
I had to ask for it. No, no I had to fight for it.
I pushed my medical team for my right have my genetics tested right around the time I was having treatment.
In the middle of chemo, I brought up the subject of gene testing to my oncologist but he dismissed me. “Tackle the cancer at hand,” he said.
“We can explore the genetics later on.”
His answer seemed logical but yet my intuition told me I needed to dig deeper.
At that point I didn’t know how finding out about the genetics side of things would affect my treatment - but I knew in my gut that knowing the results was important.
My mantra throughout my breast cancer journey is that:
Knowledge is power.
Like a child that wanted something so bad and had been told NO, from one parent, I brought up the issue again with another specialist - my breast surgeon.
Unfortunately, I also hit a brick wall trying raise the issue of gene testing with her.
My breast surgeon echoed the same sentiment as my oncologist.
Deal with the genetics side of things later on.
At that point, I decided to leave it alone. I had two specialists telling me to leave it for now.
So I decided to move on and tackle the next issue in my treatment plan. I went to seek the advice of my GP to chat about my upcoming surgery.
Lumpectomy or mastectomy?
My gut told me to go for the mastectomy. But did I dare to go against the advice of my breast surgeon? Could I have my own opinion regarding this?
My general practitioner, an older lady was empathetic to my concerns about a lumpectomy.
“Let’s get you a second opinion!” She dialed the number of a breast surgeon she had initially wanted me to see when I was first diagnosed but couldn’t because she was away on holiday. I later found out she was the breast surgeon of Australian celebrity Kylie Minogue when she had breast cancer.
Getting a second opinion with her would be a coup. If she was good enough for Kylie, she was good enough for me.
As I walked in to Miss Jennifer Senior’s office, she assumed I was there to ask for a second opinion on a mastectomy. She looked at my breast ultrasound - the tumour has shrunk to 1 centimetres. She felt my breasts and reassured me the “shadow” seen on ultrasound was just scar tissue.
I had a great response to chemo, and she thought a lumpectomy was indeed the best option for me.
I said “No no, I’m here to see if you think I should have a mastectomy instead.”
In that moment I asked another question, which flew out of my mouth and which I didn't realise was such a turning point in my quest to be heard by my specialists.
“If I tested positive for the gene, would you still recommend a lumpectomy.”
My advice for those who have concerns about their treatment,
Don’t underestimate the power of a good question. And most importantly don’t let anyone brush off your concerns. Follow that gut feeling in your stomach that senses something isn’t right. Always follow your intuition because it will always guide you to the right direction.
When a question is put forward in a certain way, it will reveal answers that you really need. And I needed the information of my gene testing to make an informed decision regarding my upcoming surgery.
At last someone was taking my concerns seriously because she told me if I tested positive, then she would recommend a mastectomy instead of a lumpectomy.
Sometimes a second opinion can be a way to educate ourselves, because most of the time we just don’t know what we don’t know.
Gene Testing and Young Women with Breast Cancer.
Results of genetic testing would normally take months to process. But because my surgical decision would be based on the results of the genetic testing, I got my results within two weeks.
Even though I was already leaning towards getting a mastectomy, I guess I needed further validation that I was doing the right thing from the genetic testing.
The testing involved a simple blood test and receiving the results was a formal consult with the genetics councillor and an oncologist that walked me through future cancer risks, screening and prophylactic surgeries.
I’m so lucky that in Australia, genetic testing is available. 7 years ago, I didn’t pay any out of pocket for my testing, although things may have changed now.
I believe that all young women that have been diagnosed with breast cancer should have genetic testing done. The earlier the better, because the results could have implications on treatment.
Testing positive was a tough pill to swallow in the beginning, and I’m not going to lie, it’s very confronting when someone is telling you about your future cancer risks. It takes me back to that movie Gattacca with Ethan Hawke where everyone has a place in society, based on their genetic makeup.
Fortunately our society is not quite there yet, but it’s a slippery slope. Insurance companies are already fighting to deny life insurance based on our genetics.
My advice is to not be scared of information. Use it to your advantage.
The more knowledge you have, the more informed your decision-making will be.
It’s also important to tell your immediate and extended family about your results. You don’t need to do this straight away, because you have enough on your plate dealing with breast cancer.
Don’t pressure pressure your relatives to get tested. Ultimately it’s their life and it’s up to them to decide to get tested. The only thing you can do at this point is inform them.
Unfortunately not all countries have genetic testing available.
Indonesia where most of my relatives live for example, don’t have access to such services. Some countries charge thousands of dollars out of pocket to get it done which some people can’t afford.
An alternative option for testing the two breast cancer genes, BRCA-1 & BRCA-2 mutations is through a the Color Kit Gene Testing Kit that you can order on Amazon for ~US$250. However, it’s important to note that other less common breast cancer genes (other than BRCA-1/2) exist, which this kit doesn’t screen for.
So you may be asking,
What’s the advantage of knowing our genetics?
Wouldn’t it just cause undue worry and anxiety knowing about our genetics? We can’t change our genetics anyway.
Well, I do worry about passing on this gene to my future kids (I didn’t have any kids when I found out). However, I believe the benefits of knowing our genetic status far outweighs the negative.
Everything is all about perspective.
It’s what you do with the information that’s important.
Here are some of the positive things I’ve learnt from having the BRCA-1 mutation.
The Positives About Having a BRCA-1 Mutation.
Did you know that studies have shown that breast cancer survivors with BRCA-1 mutation have a more favourable prognosis?
Yes it’s true!
In a 2019 study, it was also shown that breast cancer patients with the BRCA-1 mutation had a higher number of immune cells called tumour infiltrating lymphocytes (TILs). A 10% higher levels of TILs correlated to a 10% decrease in disease progression.
Most BRCA-1 carriers that do develop breast cancer are usually in the form of triple negative breast cancer. Since there’s limited treatment for triple negative breast cancer, one advantage for those diagnosed with TNBC AND BRCA-1 carriers is that there are more treatment options.
Specific Treatment for BRCA-1/2 carriers with Breast Cancers
In one study it was found that carboplatin (a platinum based chemotherapy) was superior to docetaxel in treating triple negative breast cancer patients who also had BRCA1/2 mutations.
As a result many oncologists opt to add carboplatin to the standard chemo regimen if their breast cancer patients are positive for the BRCA mutation.
There is also another therapeutic agent called poly-ADP ribose inhibitors or PARP-inhibitors that are specifically for patients who have the BRCA mutation. A number of PARP-inhibitors have been developed and their efficacy were evaluated in a number of trials involving late stage breast cancers - BRAVO, EMBRACA & OlympiAD trials.
As you know, having to deal with breast cancer is already a harrowing experience.
You feel like you have enough on your plate already.
But I found it very empowering that
as a patient, I strongly advocated for myself and I was finally heard by my doctors
as a patient, I could make an informed decision about my surgical procedure.
It’s often difficult to know if we are making an informed decision, because we rely on our doctors to tell us everything. Most of the time they will, but doctor’s aren’t fallible so there could be times where we just don’t know what we don’t know.
And the only way to remedy that is to educate ourselves and to dig deeper when our intuition tells us to.
The Four Stages of L.I.F.E. After Cancer Treatment with Coach Kylie Tolman
Life after cancer coach, Kylie Tolman talks about the four stages of life after cancer treatment. She discusses how we go through feelings of loss, insecurity, finding yourself and feeling excited about life again.
When you’re diagnosed with cancer it’s like you’re a sinking ship.
Everyone comes out to help you.
The surgeon,
The oncologist,
The hospital,
Your friends,
Your family.
They come to your rescue, fix the holes and tow your boat to safety.
The only problem is that they don’t tow you to the shore.
They only towed you to the harbour entrance and then say ‘off you go, you will be fine from here’…….
Though you are not.
You’re still adrift and everyone has gone and left you alone to find your way back.
You feel broken, exhausted, misunderstood.
Life as you knew it is no longer the same.
Your emotions are all over the place and things that used to be simple tasks, are now triggers that your brain subconsciously has stored in its memory bank that takes you completely by surprise when you least expect it.
L.I.F.E after cancer treatment is something that’s not talked about enough.
We all get to this stage in our journey and wonder what the heck is happening to us. Why aren’t we going back to life as we knew it before hand? We expect that once treatment is finished we go back to who we were before and life carries on as if it has just been on pause for a year or two while we deal with this nuisance cancer. Though it just doesn’t. We are changed forever and nothing we can do as much as we might want to, will ever change the fact that we have been on one heck of a roller coaster, our emotions, our belief systems and our fears are all different from what they were before from the experiences we have been through.
Friends and family don’t understand either.
They’re celebrating that we’ve finished treatment but we don’t feel that excitement. We feel terror and dread of the what next. What if it comes back, what if this and what if that. We’re now living in the world of what ifs and the reason is because we’ve had our world crashing down on us in a split second before, we’re afraid of it happening again as it is all soo raw and fresh in our memories.
You know what? All of these feelings and experiences mentioned above are all normal. You’re not alone for having these feelings and thoughts. In fact, I’d be surprised if you didn’t relate to at least one or two of these. They’re all part of our ‘new normal’.
Often the next part of our journey is not talked about.
But in order to move on from cancer it’s important that we’re aware and acknowledge that we go through 4 phases of L.I.F.E after treatment.
Stage 1 - Lost
Lost: This is the phase you are in as soon as treatment is finished. You’re left lost out at sea and don’t know which way to turn next. The enormity of what you’ve just been through hits you like a brick as this has been the first time you have had a chance to actually stop living on autopilot of appointments, treatments and being told what is happening next. It all catches up with you and you suddenly feel overwhelmed.
Stage 2 - Insecure
Insecure: All the raw emotions are coming up for you. You’re angry, petrified of recurrence, tired, vulnerable and no longer feeling like you as you feel like an insecure mess.
You’re wondering why you’re not going back to who you used to be.
You feel unheard and ungrateful for life.
Why have you been through all of this and not come out the other end being grateful and appreciating the small things in life like they show in the movies. What is wrong with me?
Stage 3 - Finding
Finding: You’re now ready and wanting to find who you now are. What you love. What sets your heart and soul on fire. You’re starting to understand that you’ll never be that same person you were before diagnosis and you’re ready to find and rediscover who you now are.
Finding new tools and techniques in your tool box to get you moving towards the shoreline once more.
Stage 4 - Energized
Energized: Life is starting to excite you and make you feel in control and energized once more. You’re now creating your vision of what your new YOU looks like and you feel elated and passionate about it. The days that you struggled to get out of bed every morning and look at yourself in the mirror have gone. You’ve been replaced by this new person who now has a spring in her step and doing what she loves again. This is where the fun starts!
Embracing life after cancer.
For some women these stages may take a few years to work through and others quicker. There is no right or wrong and everyone is completely different.
So don’t panic and think you’re not getting to where you want to be.
These 4 phases are a process that takes time and work and sometimes you do need to ask for help and that is ok too.
It’s important that you understand this and be gentle on yourself.
If you feel like you’re stuck and can’t get past the Insecure stage and no matter what you try it still just feels like you aren’t getting anywhere.
That’s where I can come in as the lighthouse standing on the shore to shine the light on your path and guide you back to where you belong.
I’m here to guide and navigate you with tools to increase your confidence and start living life again as the absolutely incredible person you truly are and supporting life after cancer whilst working through these phases and feeling in control.
How do I know?
I’ve walked that path.
I have walked in your shoes, with the soles wearing thin and unsure of which way to turn.
I was left adrift for years and wished I had found someone to show me the light and guide me back to shore.
I know you’re worthy and I know you can do it too.
I’m a Life After Cancer Coach who has also been through my own Breast Cancer journey being diagnosed at the age of 30 (11 years ago now). Im also a wife, mum of two boys and live in Christchurch, NZ. You can find out more about me at www.kylietolman.com
6 Types of Thoughtful Gifts That a Breast Cancer Patient Will Appreciate
If you’re at a loss to what to give someone you know that’s just been diagnosed with breast cancer, then I’ve got 6 types of thoughtful gift ideas.
This post may contain affiliate links. Please read our disclosure for more info.
When someone we know and and care about is diagnosed with breast cancer, we want to show our support. However, for someone who’s never been through cancer, it’s hard to know what a woman with breast cancer needs.
If you want to send gifts that are more thoughtful than a bunch of flowers then read on because I will be giving you 6 gift ideas that can make a cancer patient’s journey easier.
1) Planning to Thrive
Once a woman is diagnosed with breast cancer, she has so many important things to remember and write down, such as specialist appointments, scans, tests and treatment appointments are just a few things that she needs to track of so having a dedicated journal to manage the practicalities of dealing with cancer can be extremely useful.
Canplan is the best organizer for cancer patients and is the perfect gift for someone who is newly diagnosed. This journal allows the cancer patient to have a holistic approach to fighting cancer. Some of the features worth mentioning are the appointment tracker which has space to write down things like questions to ask the doctor, notes to take during the appointment etc. Patients can also track any side-effects they experience so they can confidently remember to relay the details to their doctors.
It also has positivity exercise to help the mental side of things, tips for healthy living and much more. You can check it out HERE.
2) Moving to Thrive
Exercise has been shown to be the best way for cancer patients to minimise the side-effects of cancer treatment and to avoid a recurrence. However, a depressed immune system during chemotherapy means they might not want to go to their local gym to do a workout.
Encourage them to keep active in the outdoors or do some indoor exercise like yoga in the comfort of their own home. You can buy an awesome yoga mat like this one that includes a personalised message.
Gone are the days of having to buy exercise videos only to be bored of them shortly after. Instead, opt to stream endless variety of high quality exercise videos from YouTube - totally FREE. There’s many channels offering yoga, pilates, barre, cardio boxing, zumba, dance, hip hop etc.
The key here is to use a push device like the Apple TV to turn a humble living room into a private exercise studio. You can check it out HERE.
Using a push device like the Apple TV allows you to watch or listen to any media that is playing on your IOS device or mac computer onto your big screen TV. My favourite way of working out at home is to browse the endless selection of YouTube workout videos (totally freeee!) on my phone and push them onto my cinema screen essentially turning my living room into an exercise studio. It’s perfect when you’re housebound and still want to exercise. Most exercise routines don’t need a lot of space and as long as I can fit a yoga mat, then I find I have enough room.
3) Head Covering
If chemotherapy is in the treatment plan then the cancer patient will most likely experience hair loss. Good quality, natural looking wigs can be expensive so if you know that she’s planning to get a wig, consider chipping in the expense in the form of a gift certificate to a wig salon.
Wigs can get hot, itchy and uncomfortable, so she won’t be able to wear it 24/7. It’s also important to have a variety of comfortable head coverings especially during winter when it’s very cold to go out bald or sleep with an uncovered head.
A head cover made out of soft stretchy fabric would be ideal like this one.
In summer, satin or silk is the best fabric for a bandana because it’s cool, soft and light to wear on the head. Check out this large selection of satin/silk scarves in many different colours and patterns HERE.
4) Books to Make the Journey Easier
One of the best cancer gifts I received were books about what to expect after a breast cancer diagnosis. Some great books that make navigating a breast cancer diagnosis and treatment easier include:
The Silver Lining: A Supportive and Insightful Guide to Breast Cancer
Just Get Me Through This! A Practical Guide to Coping with Breast Cancer
If the patient has indicated that she’s wanting to a more healthier lifestyle, then these books can be perfect gifts for her.
Memoirs about surviving cancer can also be a good read. They are usually personal, entertaining and inspirational. It can give a different perspective to a difficult journey from someone that has gone through it all.
Some great books include:
5) Give the Gift of Nutrition
If your loved one seems motivated to live a healthier lifestyle after her breast cancer diagnosis then you can support her health and wellness journey by contributing to the tools she needs.
You can get her started on juicing by getting this book by Kris Carr, a long-term stage 4 cancer survivor.
And if you want to totally spoil her you can purchase a good quality cold-press juicer which retains more vitamins than conventional centrifugal juicers.
If you’re more worried about what she eats when she’s too sick to cook for herself or her family then help her out by dropping off some nutritious meals on her doorstep. If cooking isn’t your thing then you can look out for a meal service that delivers good quality nutritious food.
For a gift that she can use long-term then a good quality steamer can be a really good gift option that she can use even after her treatment is over. Steaming foods retain a lot more vitamins, minerals and nutrients in food than any other methods of cooking such as baking, frying, boiling and stewing.
6) Give the Gift of Laughter
A cancer patient has lots of free time to recuperate from cancer treatment, especially when she has taken time off work. A Netflix subscription can be a great gift idea, because there’s lots of funny movies and stand-up comedy shows to choose from that will make her laugh.
Going through cancer can be an extremely stressful time for the breast cancer survivor and their families. By giving them a good dose of laughter, you can help ease the tension and forget their troubles - even if it’s for a short period of time.
Other ideas include a cute cat sock like this one that will make her chuckle.
… Or a totally inappropriate adult colouring book like this one.
It’s never too late to give a gift to a cancer survivor. If you haven’t been in touch for a while since her diagnosis, then explain to her honestly and truthfully. Sometimes we don’t know what to say to someone that’s just been diagnosed with cancer, but at least after reading this post you’ll know exactly what to get her and show how much you care.
The Art of Thriving with Cancer- Part I: How to Feel Confident in the Face of Uncertainty
If you're struggling to keep it together after a cancer diagnosis then you need to read this post. I talk about four key areas that you need to focus on in order to increase your confidence that you'll beat cancer, so you can keep on moving forward and tackle the problems that lie ahead of you.
Too much certainty in life makes us feel bored.
Too little certainty, and we spiral into anxiety and panic.
For those of us given the cancer card, uncertainty becomes a constant companion. We don’t know if we’ll be here tomorrow, in a month, or in a year — and that thought alone can make us double over in fear.
Of course, no one really knows how long they have. Any of us could be hit by a runaway bus tomorrow. But we don’t think about that every day. With cancer, we do.
The Exhaustion of Living in “Maybe”
After diagnosis, every day becomes filled with questions:
What if the treatment doesn’t work?
What if tomorrow is the day it comes back?
What if I never get the all clear?
The waiting feels endless. One, two, five, ten years of holding your breath until you can exhale. Living in this state isn’t really living — it’s existing, enduring, barely moving forward.
No wonder panic attacks, breathless anxiety, and sleepless nights become so common.
Why Fear Shows Up After a Cancer Diagnosis
Here’s the truth: we will never live a life without fear. Once diagnosed, that fear is always there — sometimes as a roaring flame, sometimes just a faint pilot light.
Fear’s job is to protect us. The problem is, it often oversteps. Instead of keeping us alert, it paralyzes us. We go into defensive mode. Some of us even curl up in the fetal position emotionally, vowing never to be blindsided again.
But here’s the shift: you don’t need to be disappointed in yourself for being scared. Fear is human. The key is learning how to live alongside it, without letting it dominate your every step.
The Hardest Part: Starting from Zero
The start of the cancer journey is always the hardest.
Your confidence is blasted to ashes. You don’t trust your body, your health, or your future. You feel like you’re standing at ground zero, unsure if you’ll even make it.
But like anything hard in life, the only way forward is small steps. Quivering, shaky steps at first. But step by step, confidence grows.
Nobody wakes up with a full tank of confidence. It’s built — layer by layer, win by win.
👉 Pro Tip: Start celebrating your small victories, no matter how tiny. Each one becomes a building block for confidence, and slowly the fear loosens its grip.
The Two Battles You’re Really Fighting
Every cancer journey has two parallel battles:
The Body Battle – fighting the disease with treatment.
The Mind Battle – fighting despair, fear, and hopelessness.
Both matter. Both deserve your attention. And thriving means taking your mental battle seriously, not treating it as “secondary” to the physical one.
The Four Pillars of Confidence
Over the past fifteen years since my diagnosis, I’ve discovered four core areas that shape whether you feel stuck in fear…or confident enough to thrive. Conquering these four factors will help you move forward with poise, grace and dignity - despite what the outcome will be.
Your Beliefs – Your unique experiences, memories, and emotions create the lens through which you see the world. They shape your self-talk.
Your Mindset – What you choose to focus on daily is the biggest game-changer in how you tackle challenges.
Advocating for Yourself – Speaking up with your healthcare team ensures your concerns are heard and your choices respected.
Your Healing Journey – How you recover, rebuild, and redefine your “new normal” determines how you move forward.
These are the four pillars of confidence. Strengthen them, and you stop just surviving — you start thriving.
I’ll dive into each of these pillars in my next post, but here’s the most important reminder: confidence doesn’t appear all at once. It’s built slowly, win by win.
Trifina Sofian is a life coach specialising in cancer recovery and mindset management. She helps cancer survivors be in the best state of mind to beat cancer and maximise their healing potential. Trifina can help you reprogram your mind to conquer cancer and help you build a more positive state of mind and body. Check out her new book Win the Fight Against Cancer - How to Master the Mental Battle HERE.
Harness the Power of Facebook Groups to Help You Beat Cancer
I wish I’d known about Facebook groups. Getting diagnosed with breast cancer in my late 20s was extremely lonely. I had to miss out on big family events like my sister’s wedding overseas because I was in the middle of my chemo treatment and too scared to catch a flight because of risk of infection. So while my family was celebrating, I was busy stressing out about pumping up my veins so the nurses can easily insert the cannula on chemo day. While my friends were busily going about their day at work, I was stressing out whether feeling breathless was a sign that I had a blood clot in my lungs.It totally sucked.
I wish I’d known about Facebook groups.
Getting diagnosed with breast cancer in my late 20s was extremely lonely.
I had to miss out on big family events like my sister’s wedding overseas because I was in the middle of my chemo treatment and too scared to catch a flight because of risk of infection.
So while my family was celebrating, I was busy stressing out about pumping up my veins so the nurses can easily insert the cannula on chemo day.
While my friends were busily going about their day at work, I was stressing out whether feeling breathless was a sign that I had a blood clot in my lungs
It totally sucked.
It felt like everyone in the whole world was living a carefree existence and I was the only 20 something woman that ever existed having to deal with breast cancer.
It felt like the whole world continued on living, while I got left behind.
I wished I had known there were other young women battling through breast cancer. Knowing other people were walking the same uncertain path - struggling the same struggles, feeling the same fears would have helped - ALOT.
There’s something to say about strength in numbers.
Last year Mark Zuckerberg announced that he was going to “Bring the world closer together”. His goal is to “bring one billion people to join meaningful communities” via facebook groups.
Having a community can make us feel less afraid, that there’s something bigger than just us and that there’s something to look forward to.
But 8 years ago when I was first diagnosed, I don’t even think Breast Cancer Facebook groups even existed, so I think you’re lucky that today, the technology has allowed us to come together in solidarity.
Everyone’s on Facebook
The biggest advantage between Facebook groups versus the traditional online cancer forums is the convenience and the number of users in the platform. Today, there are 2 billion people on Facebook.
You can access Facebook via the app so much easier on your phone.
Think about how often you would update your FB status and check your newsfeed?
Therefore, it’s extremely convenient for people to join and actively contribute to the conversations that are happening in Facebook groups.
Online forums on the other hand are usually hosted on a website that you need to register and login every time you want to connect to these communities - making them cumbersome, so you don’t go on it as often.
When I was diagnosed, I joined a small online breast cancer forum but because I was young and diagnosed with a less common form of breast cancer, I felt like I didn’t fit in to that particular online space.
Getting Started with Facebook Groups
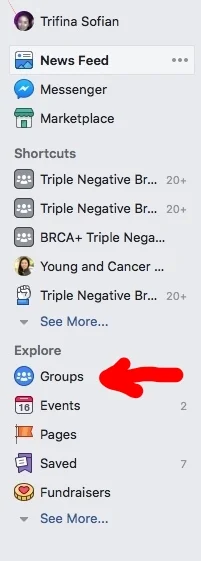
So what do you need to do if you want to join a cancer Facebook group?
Firstly, you need to search for a group that is most important to you.
To figure this out, you need to ask yourself some questions. Some examples:
Is location of the people in that group important to you?
Do you have specific questions regarding your own specific breast cancer?
Are you struggling with a particular type treatment?
Are you apprehensive about deciding on a surgical procedure?
To give you some ideas of the types of breast cancer facebook groups out there, check out the table later on this post.
If you’re on desktop- You can search for groups on the left hand column in the “Explore” section.
If you’re on the facebook app - You can search for groups by clicking the more section in the bottom right hand corner of your screen and click on “groups”
All you have to do to get started is find a group you want to join. Because these groups are private, usually the moderator will set some questions that you need to answer to make sure that you really belong to that particular group before getting accepted.
Some cancer facebook groups can range from a few people to tens of thousands.
So what do people post about in these groups?
People can post about their feelings and thoughts in these groups. It’s a great way to vent and let out the emotional stuff that comes with being diagnosed with cancer.
In the bigger groups, with thousands of member from all over the world, you’ll get a response to your burning question within a few minutes after you hit post.
Wanna know if your weird symptom is normal after your first treatment?
Someone’s there to tell you they’ve experienced it too.
Going outta your mind waiting on the results of your most recent scan?
A reassuring message will pop up telling you “It’s all going to come back clear.”
Celebrating a small milestone in your treatment plan?
Someone’s there to give you a virtual hug and high five.
Finding People in the “same boat”
No one really wants to be part of the C-club.
But finding a group of people that can empathise with you after a life altering diagnosis can make you feel less alone - that you’re not the only person going through this crappy journey.
We all want to be heard and we all want to be understood.
However, your situation and your pathology is unique to you, and no one is going to be in exactly the same “boat” as you.
The great thing is you’re not limited by how many Facebook groups you can join.
Whatever challenge you’re facing, there’s bound to be a group for it.
To show you how much choice there are, I’ve listed a few breast cancer facebook groups as examples to the breadth of communities.
Check out all these different Facebook groups.
Hearing a Different Perspective
When we’re diagnosed we’re bombarded by information that we find confusing and medical jargon that we don’t understand.
Your private community can get you up to speed with the lingo, and clarify anything you’ve found confusing during your consult and even suggest further questions you need to ask.
I think this is fantastic as the more we’re able to understand our disease and treatment, the more informed and empowered we are of our journey.
Difficult decisions also need to be made along the way. Having an online community that you can use as a sounding board for your thought process can be helpful.
Hearing different perspectives from people who have gone through it all before, can suddenly bring clarity to your own decision making process.
But I think the most powerful thing Facebook groups can provide us access to cutting edge new information regarding testing or treatment. This includes such things like clinical trials that’s being conducted around the world. You’ll get clues to how people are responding to these cutting edge treatment.
This is even more critical if you've been diganosed with Stage IV metastatic cancer and you need to be thinking out of the box and look into more experimental methods of treatment.
It’s hard to keep pace with medical research and by the time results hit the news, it might be old news already.
Remember, it’s important to understand that we need to be getting the BEST medical care - not just medical care that your doctor is familiar with.
Some Things to Be Aware Of
Before you post anything to these groups, it’s important to realise that each group has a set of culture and values. This is usually set by the admin or the collective users themselves.
Read and try to understand the rules. There’s also bound to be some unwritten “rules”. Pay attention to what the admin and moderators of that group posts. This should give you some clues of the do’s and don’ts, otherwise you might run the risk of getting kicked out.
For example, one of the groups that I’m a member of don’t support the exclusive use of natural cancer cures to treat cancer.
So asking questions about natural remedies is a “no-no”.
Another big downside to joining Facebook groups is you get to see reality of cancer.
You’ll read stories of recurrences and members gaining their wings.
As you can see, there’s so many benefits in joining private facebook groups, however, giving back to these communities is essential for the whole group to thrive.
But ultimately you must do what’s right for you. If it all gets too much you can turn notifications off in these groups and come back again or exit the group permanently.
I personally joined these breast cancer facebook groups to let others starting this journey know there are long term survivors so they can feel inspired to keep moving forward.
If you found this post useful, please comment down below and let me know how facebook groups have benefitted you in your cancer journey.
9 Simple But Effective Ways to Maximise Chemotherapy While Minimising Side-Effects
In today’s post, I’m going to share with you the things I did during chemotherapy that allowed me to achieve a complete pathological response and how I also breezed through chemo with minimal side-effects. I also digged deeper into some of the studies looking at how to increase the effectiveness of chemotherapy which you may wish to implement during your treatment.
This post may contain affiliate links. Please read our disclosure for more info.
Out of the three cancer treatments, going through 6 cycles of chemo was the most grueling and physically challenging part of surviving cancer.
A mastectomy and radiotherapy? Those felt like a walk in the park.
When I found out I had cancer, my breast surgeon recommended I do chemotherapy first—neo-adjuvant chemotherapy, meaning chemo before surgery.
I was in such shock in the beginning that I didn't question whether this was the right thing to do. Luckily for me it was, because here I am 15 years later, alive and well.
I had survived triple negative breast cancer.
Having a receptor-negative breast tumor meant that chemotherapy was especially important—it was the only systemic treatment available for me at the time.
My main concern was that any microscopic cells that had potentially broken off from the main tumor and floated around in my blood could "seed" the spread of cancer to my vital organs.
Having a lump in my breast wasn't the thing that was going to kill me. It was the spread into the major organs that would be the tipping point. So I had to embrace my chemo treatment like my life depended on it.
There was no back-up immunotherapy or hormone receptor blockers for me after I finished treatment.
I needed the chemo to work.
So I decided I had to give it all I've got. I did what most people didn't think of or weren't willing to do.
And boy did it pay dividends!
I had a complete response to chemo.
Here's the thing most cancer patients don't realize: You're not as powerless as you think.
While you can't control having cancer, you CAN control how you prepare for treatment. You can be strategic instead of passive. You can be the CEO of your healing journey instead of just patient #47.
That strategic approach? I've turned it into a simple system you can use - The 48 Hour Chemo Power Protocol.
So before we get into the 9 tips make sure to download your free protocol checklist.
One important thing to note before I share with you my tips is that if you’re having neo-adjuvant chemotherapy (having chemo before surgery), then the best possible outcome from finishing your chemotherapy is what physicians call a complete pathological response. This means that the chemotherapy you received was effective at killing 100% of the tumour in your breast and/or lymph nodes.
The only way you’ll be able to know if you had a complete pathological response is if you had chemotherapy before you have breast surgery.
Having chemotherapy after the tumour has been removed from your body makes it impossible to know whether the chemotherapy was effective at killing any stray cancer cells. You will have to rely heavily on your faith that the chemo had done it’s job at wiping out all the cancer cells in your body.
What also surprised me (many years later) was when I heard about women who had the same cancer I had, but didn’t respond to the same chemo regimen that I received.
Their tumours didn’t shrink at all and in fact some of their tumours grew in the months that they were in active chemo treatment.
So be wary that if you’re having neo-adjuvant chemotherapy you need to be confident that your treatment is working. If your tumour isn’t shrinking, then a change in treatment strategy is needed ASAP.
📍Pin for later
In today’s post, I’m going to share with you the things I did during chemotherapy that allowed me to achieve a complete pathological response and how I also breezed through chemo with minimal side-effects.
I also digged deeper into some of the studies looking at how to increase the effectiveness of chemotherapy which you may wish to implement during your treatment.
Chemotherapy directly kills cancer cells in your body, but the downside is that it’s non-targeted meaning it can’t differentiate between cancer cells and normal cells. So you might be killing some cancer cells but it’s also likely harming your normal healthy cells - which is why you may experience some side-effects during chemo.
When you’re feeling unwell and icky from chemo, the natural tendency is to lay around and do nothing.
So how do you mitigate some of the serious side-effects of chemotherapy?
The answer is to also nourish and protect your normal healthy cells.
If you experience serious side-effects during chemotherapy then your oncologist may warrant stopping treatment early - decreasing your chances of achieving a complete pathological response.
So when you’re having chemo, your goal is to be able to finish ALL the sessions of chemotherapy that have been planned by your oncologist, and the best way to do this is maximise its effectiveness while minimising side-effects.
One of the main side-effects of chemo I was concerned about was nausea. Generally, I’m a queasy kind of girl and can go green very easily, so naturally I was super worried about vomiting.
However, my oncologist assured me that in this day and age, the anti-nausea drugs are so good, that no cancer patient should be vomiting whilst on chemo, otherwise they need to go back to their doctor and demand to change their anti-nausea medication.
This was so reassuring and I was very pleased to not vomit once during the six cycles of chemo I had.
I found it really disappointing that my oncologist didn’t give me ANY “lifestyle” tips about what to eat or what to do during the months that I was having treatment. I soon realised that most oncologist are not really trained or have any real interest in nutrition or holistic healing.
I think as cancer patients, we need to be more proactive about our recovery. Just because our oncologist hasn’t mentioned anything about what to eat or other lifestyle things, it doesn’t mean that we can’t focus on adopting “extra” healthy initiatives, as long as we’re open with our oncologist about what we’re doing whilst on chemo.
It was only recently that the Australian Society of Oncologist released a statement advising the benefits of exercise during chemotherapy to combat side-effects, even though the evidence has been building up for many years.
For most of us, we’re battling cancer right now so we don’t have the luxury of waiting for the medical community to slowly adopt new and beneficial things.
Because I bounced back relatively well after each round of chemo, getting involved in my own recovery also had huge benefits of increasing my confidence and empowering my mind.
It made me feel less helpless in this roller coaster of a cancer journey.
I had something to do and something to focus on every single day.
So in today’s post, I want to share with you my top 9 tips for chemotherapy.
The tips I’ve mentioned here are simple and doable with a bit of preparation. Full disclaimer, to double-check with your oncologist before adopting any of the things I’ve mentioned here.
Tip #1: Weaken your cancer cells and protect your healthy cells through fasting
At the time of my chemo treatment 15 years ago, I hadn’t heard about the benefits of fasting, however, today it’s gaining popularity.
So how does fasting work to benefit us during chemo?
The benefits of fasting has been shown in animal studies and is two-fold.
Fasting increases the effectiveness of chemotherapy and also reduces its toxicity.
It’s thought that during fasting, healthy cells don’t spend energy on growing but instead they spend their energy in a “protective” state. Cancer cells don’t do this during fasting - a term called differential stress resistance.
How long should you fast for?
That’s a good question and we’re not really clear on the duration. There are only a few human studies to date (1, 2) but they have all been very positive.
In a 2018 study of 34 women with either breast or ovarian cancer, the duration for fasting was 36 hours before chemotherapy and 24 hours after. It was found that the women tolerated the fasting quite well and seemed to improve their quality of life such as fatigue and gastrointestinal symptoms compared to when they didn’t fast during chemo. During the fast they were allowed only water, herbal tea and a small amount of vegetable juice or vegetable broth. You can find more details of the study here.
If you are thinking of doing fasting during chemotherapy, just make sure you inform your oncologist and point them to these studies I’ve mentioned.
Tip #2: Up your level of nutrition through juicing
Alot of women will gain weight during chemotherapy, probably a contrast to what most people believe. This could be because of stress and emotional eating or it could be due to the steroids they’re given by their oncologist to dampen down any allergic type side-effects.
In any case, it’s important that you stick to healthy meals when you’re not fasting. A cooked plant based diet is easier to digest and kinder to your gastrointestinal system - which will be severely compromised during chemotherapy. Because the lining of your gut replicates quite quickly, the chemo - which affects rapidly dividing cells -will wreak havoc on your digestive system.
I believe, the quickest and most effective way of getting nutrition into your body is through juicing. I started juicing as soon as I was diagnosed so I had a few weeks of absorbing liquid nutrients before I started chemo.
I juiced a lot of fruits and vegetables. It was mainly carrots and spinach in the beginning and later on I cut down the carrots due to the high sugar content and added more cruciferous vegetables like broccoli and cauliflower.
When you’re having chemotherapy, stock up your fridge with lots of fresh fruits and vegetables. Invest in a good quality cold-press masticating juicer because they retain more vitamins and nutrients than conventional juicers which shreds and oxidises the nutrients.
Juicing should really be one of the thing that you focus on during chemotherapy. It hydrates you, deliver loads of nutrients and detoxifies your body.
Favourite juicer: Omega J8006HDS
Tip #3: Increase your circulation
The aim of chemotherapy is to kill any floating cancer cells in your circulation. These cells can act dormant for many months or years and as I’ve said before, it can “seed” the spread of cancer to other organs. Therefore it’s vital to kill all rogue cells that may be present in every nook and cranny of your body.
To do this, I think it’s important to open up your blood vessels and maintain good circulation just before you start your chemotherapy infusion, during the infusion and afterwards when you get home.
During the day of infusion, I would do a short workout at home or I would walk to the hospital where I was having my treatment. It was only 15 minutes away so it was great preparation before going into my infusion session.
If you don’t live near the hospital, you can also try to arrive early on the day of your infusion and go for a brisk walk around the grounds of the hospital. Breathing in lots fresh air and getting your blood pumping is a great prep before you go in to the hospital both physically and mentally.
A quick check that you have good circulation is to see that your hands and feet are warm and pink.
I also placed a warm heat pack on my chest where the tumour was located. The infusion would typically last a good few hours, and I always made sure I covered myself with warm blankets for the entire duration, never getting cold even with the air conditioning blowing around me. This ensured the chemo would freely flow to all parts of my body that cancer could be lurking in.
**Bonus Tip: As the chemo is flowing into your veins try to relax, breathe deeply, close your eyes and do some meditation and visualisation. I like to visualise the chemo drugs dissolving all the cancer cells and disappearing to nothing.
Most of the oncology wards now provide cold-caps for their patients to preserve their hair. Although losing my hair was one of the most traumatic things I had to endure, I don’t think it’s worth doing because my intuition says that it could affect the effectiveness of chemotherapy.
The reason I say this is because of the way it works.
Cold-cap decreases the blood circulation on your head and thus reducing the effectiveness of the chemotherapy at killing the hair follicles. If your hair-follicles could be spared then that means any cancer cells in the vicinity could be spared as well. It only takes one single cell to form a new tumour and that’s why I caution the use of cold-caps just because I think it can potentially compromise your circulation during treatment. In my opinion, it’s not worth it. Hair grows back. Focus on what’s important - killing cancer cells.
Tip #4: Expel the toxins out
After the chemotherapy has been pumped into your body, it’s important that you’re able to effectively pump it out, so your body can recover and be ready for the next session.
So don’t forget to hydrate! Drink lots of fluids like your life depends on it so you can pee out all that extra chemo out of your system ASAP.
Maintaining really good blood flow and circulation is equally important after your session is over. Now that you’re recovering at home, your liver will be in overdrive trying to detoxify the chemo that’s circulating in your blood.
You might be feeling pretty crook for the first few days after your chemo session and that’s perfectly normal.
For the first few days, sometimes getting out of bed would be a huge challenge.
I would peel myself from my comfy bed and just walk around intermittently in circles in my tiny apartment. I would go back to bed and repeat throughout the day.
Sometimes I would feel too out of it to walk around the block, so my husband would hold my hand and we would walk together. Getting some fresh air actually felt really good.
The key here is to move your body as much as you physically can to maintain good blood flow to your liver.
When I was feeling much better I would exercise vigorously. This is another critical component to why I believed I responded so well to the chemo while minimising side-effects.
Sweating is a fantastic way to detoxify your body.
When you feel like you’ve recovered well enough after chemo, you have a short window of opportunity to up the intensity of your exercise regime before another round of chemo will hit you again. So it’s critically important that you make the most of this time to do a full body workout.
Tip #5: Hydrate, hydrate, hydrate!
It’s extremely important to hydrate before, during and after your infusion. I would also supplement with some fibre on the day of treatment and several days after to avoid severe constipation which most women will suffer due to the chemo drugs and the anti-nausea drugs. My favourite fibre supplement is this one.
Before I left for the hospital I would usually prepare a big jug of water or liquids next to my bedside table so when I got home I could just crash in bed, and it was there ready and waiting for me to hydrate.
In chinese medicine, it’s believed that chemotherapy is “heaty”. It’s the reason why you experience “heaty” symptoms such as mouth ulcers, constipation and flushing. In order to counteract the “heatiness” we must eat or drink some “cooling” foods or liquids. So other than water next to my bedside table, I also cooked a big pot of pearl barley and drank the cooled water that it had been boiling in.
I also drank a pot of chrysanthemum tea if I haven’t opened my bowels the next day.
Because I was so well hydrated and supplemented my liquids with some fibre, I didn’t have any issues with constipation and never needed to take any laxatives.
Tip #6: Bolster your immune system
Even though you’ll be given an injection to increase your white blood cells, your immune system will still take a big hit during chemo.
It’s important to avoid a serious infection whilst on treatment because this can delay your next cycle. Avoid being around sick people and because we all can’t live in a germ-free bubble, it’s important to strengthen your immune system.
Eat foods that support a strong immune system.
Once you’ve finished chemo, your immune system will be at its weakest and yet, that’s when you need it to be the strongest as it’s the main factor in keeping you cancer-free in the long-term.
Asian mushrooms like maitake and shiitake are great immune boosters. Saute them in some garlic, another immune boosting food.
In Japan, these mushrooms are served in hospitals where patients are undergoing chemotherapy. They contain a molecule called letinan. You can find these in your local oriental grocery store but if there’s none near where you live, then the next best things is to take a mushroom and immune boosting supplement like this one. Some asian mushrooms like reishi can’t be eaten fresh and you must take them in a capsule.
RELATED ARTICLE: My Top 10 Evidence-Based Anticancer Supplements
Tip #7: Revive and protect your healthy cells
Eating really well during treatment is important to provide your healthy cells with loads of antioxidants that keep it protected. Munch on lots of anticancer fruits like berries and cooked vegetables especially the cruciferous ones like broccoli and cabbage.
Keep up the fresh juices, they will nourish and hydrate you at the same time.
Lastly, invest in some supplements to further protect your healthy cells from radical damage caused by chemo. However, it’s also important to not have too much antioxidants when chemo is still circulating in your bloodstream - which is usually 24-48 hours after your infusion. You don’t want to cancel out the effects of the chemotherapy by having too much antioxidants - it really is a delicate balance.
I talk more about my supplements regime here in this article.
Tip #8: Rally support
I had my infusion every three weeks for a total of 6 infusions. What’s really important to emphasise was how regimented I was during those couple of months on chemo.
I can’t take full credit for this as my husband was the one that prepared everything for me and was constantly reminding what I needed to do.
If you have a support person to take care of you during chemo, then it’s a good idea to show them this article, so they can better prepare and assist you during chemo so all you need to focus on is recovering.
I would highly recommend that you also join a support group - online or real life. One of the big benefits of support groups - especially if you join one that has hundreds or even thousands of members, is that someone will answer your questions pretty much straight away.
They can provide you with helpful and practical advice when you’re struggling with the side-effects of the chemotherapy.
Tip #9: Boost your mood
It’s vital to keep your spirits up during the many months it would take for you to complete chemotherapy. Try and see your friends and family during your treatment so you won’t feel so isolated.
Watch some funny movies on Netflix to take your mind off the mental and physical stress you’re experiencing.
Keep a journal and write your feelings down. The health of your mind is just as important as your physical body during treatment.
Remember that laughter will release feel good endorphins. It really is the best medicine when you’re feeling crap.
Lastly, don’t forget to celebrate the end of your chemotherapy. Compared to surgery and radiation, chemotherapy is by far the hardest treatment to physically and mentally endure.
Trifina Sofian is a life coach specialising in cancer recovery and mindset management. She helps cancer survivors be in the best state of mind to beat cancer and maximise their healing potential. Trifina can help you reprogram your mind to conquer cancer and help you build a more positive outlook and life. Check out her new book Win the Fight Against Cancer - How to Master the Mental Battle HERE.
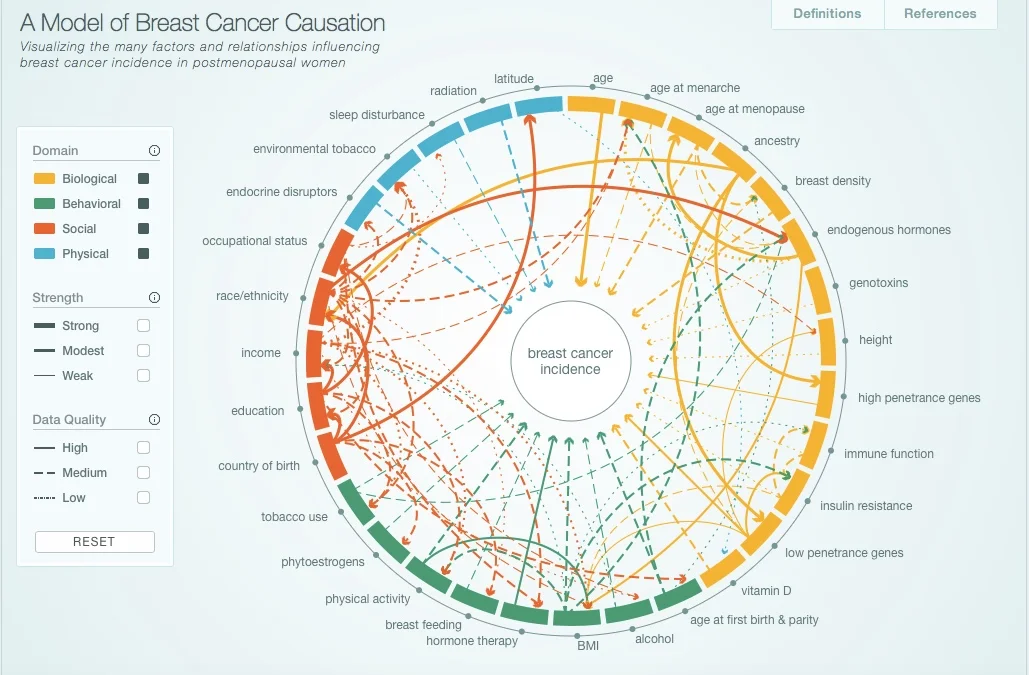
What Causes Breast Cancer? The Risk & Real Factors You Need to Know
Most women think that getting breast cancer is bad luck. This is false and what's even worse is that oncologists are spreading this false statement simply because there is no universal cause of breast cancer. In this post I look at the current evidence on the risk factors in order to gain understanding, can better assess and minimise our own risk factors for breast cancer. If you have a family history or you're looking to reduce a recurrence then this is a must read article
This post may contain affiliate links. Please read our disclosure for more info.
"It was just bad luck, so don’t blame yourself,” my oncologist explained.
I knew in my gut it wasn't "normal" for someone in their 20s to develop breast cancer. Not that getting cancer at any age is acceptable.
I thought hearing my oncologist's explanation of why I developed breast cancer would put everything in perspective. But blaming this on bad luck seems so -- unscientific.
I had a burning question ever since I was diagnosed:
Is breast cancer really random?
Having a background in science, I knew there’s more to getting breast cancer than bad luck.
The Incidence of Breast Cancer is Rising
October is breast cancer awareness month and the “pink” campaigns will soon surround us promoting early detection, breast screening and seeking donations to fund a cure.
What’s really hard to believe is that we have yet to see an improvement in the incidence of breast cancer.
Have you ever noticed the lack of prevention campaigns for breast cancer?
It’s crazy to think that after billions of dollars spent on breast cancer research, there’s never been any major breast health campaign. There’s lots of awareness in checking your breasts and being wary of early signs and symptoms.
But isn’t stopping it altogether better than catching it early?
So what do the experts tell us about the cause of breast cancer?
If you haven't already checked out any of the respected breast cancer organisation websites, they all state risk factors that increases the chances of a woman developing breast cancer (see table below).
These risk factors are divided into UN-MODIFIABLE (those that you can't change) and MODIFIABLE (those that you can change). There’s also evidence that a few protective factors decreases the chances of a woman developing breast cancer. Check out some of the most common risk factors below.
Those risk factors seems pretty straightforward.
But in simply visualising the risk factors as neat bullet points, we’ve lost appreciation of the intricacy of what causes breast cancer.
There is a more complex picture.
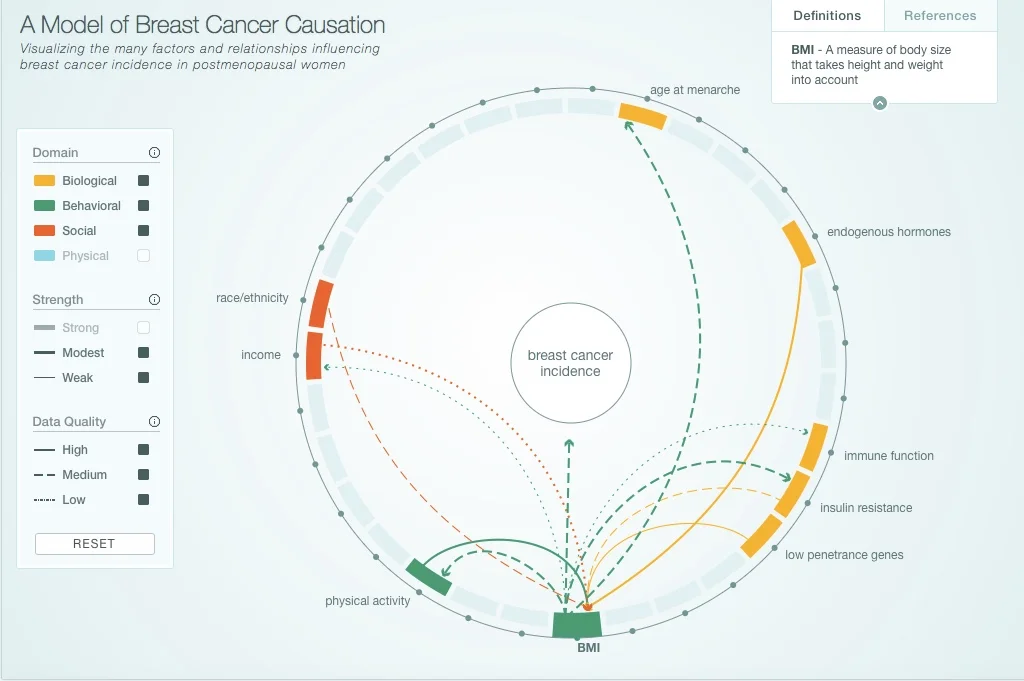
We can begin to understand this in the model of breast cancer causation created by Robert Hiatt from the UCSF.
In this model, the development of breast cancer is an interplay of risk factors that fall under four major categories:
Biological
Behavioural
Social
Physical
The research gathered has been from postmenopausal women and are currently working on a similar model for premenopausal women.
I recommend you click through to their website to play around with their interactive model to educate yourself on how one risk factor are connected with other risk factors.
Interactive Model of Breast Cancer Causation - http://cabreastcancer.org. The full research article was published in journal Cancer Epidemiology, Biomarkers and Prevention can be found here.
If you click on just one risk factor, for example BMI (see screenshot below) - it displays any relationships with other risk factors:
physical activity
race/ethnicity
income
age at menarche
endogenous hormones
immune function
insulin resistance
low penetrance genes
However, as you can see there are different lines connecting them, and they differentiate between the strength of association and the research data quality.
Unlike cervical cancer that’s caused by human papilloma virus (HPV), and most incidence of lung cancers are caused by tobacco smoking, the cause of breast cancer isn’t as straightforward.
It’s far more complex.
And here comes the confusing part…
Having one or more risk factors doesn't mean a woman will guarantee to get breast cancer.
And...
Many women who DO develop breast cancer have no obvious risk factors.
How do we make sense of this?
Firstly, I think it’s important to realise that the cause of breast cancer EXTENDS BEYOND these published risk factors.
If you’re at all concerned about preventing breast cancer or if you’ve already been diagnosed you need to understand these risk factors in the context of your own circumstance.
The Real Factors that Causes Breast Cancer
What isn’t explained in great detail is the fact that there is a common underlying reason why these risk factors have been associated with breast cancer.
The majority of these risk factors directly and indirectly relate to oestrogen dominance.
Let’s look at some of these risk factors again:
younger age at onset of menstruation and older age at onset of menopause exposes the woman to a longer duration of circulating oestrogen.
Consuming alcohol impairs the liver to metabolise oestrogen.
Having a high BMI means having a greater amount of fat cells that are able to produce more oestrogen in the body.
Being on the contraceptive pill means adding exogenous oestrogen into the body.
Being on HRT means adding exogenous oestrogen into the body.
Having children earlier on in life and having more than one children is a protective factor, because pregnancy interrupts the levels of oestrogen in the body.
Normal breast cancer cells contain oestrogen receptors and when oestrogen binds to these receptors, it tells the cells to grow. If a breast cell has been damaged by radiation or toxic exposure, having excess oestrogen around will allow the “bad cells” to flourish and grow.
But usually the immune system of young women are able to take out these bad cells. However, when a woman’s immune system becomes weak for long periods of time, these single cancer cells can grow into a tumour.
What’s the association of oestrogen and triple negative breast cancer?
The concern with oestrogen dominance still applies.
Even though oestrogen doesn’t fuel the growth of triple negative breast cancer, you have to remember that before it turned into cancer cell, it was once a normal breast cell with oestrogen receptors.
We also need to educate ourselves about the impacts of toxins, radiation and pollutants on breast health. A woman’s mammary glands are surrounded by fatty tissue. We all know that toxic chemicals accumulate in the blubber of whales and dolphins.
The high levels of toxins that build up in the fatty tissue of the breast which are in close proximity to breast cells initiate the DNA errors that lead to cancer.
What does the complex interplay of risk factors look like in real life?
Let’s take my development of breast cancer as our case study.
Women like myself who have inherited a faulty BRCA-1 or BRCA-2 gene have an impaired DNA repair mechanism in their breast cells.
So how do you explain young women that develop breast cancer who’ve tested negative for any BRCA mutations?
The number of breast cancer associated genes are expanding. Perhaps these women who’ve tested negative do have mutations in several subtle genes. And the likely explanation is that we haven’t identified all the genes responsible for maintaining normal breast cells. There’s no doubt that BRCA-1 and BRCA-2 are the single most important genes identified to date.
However, it’s important to go back to the fundamentals.
There’s more to breast cancer development than one faulty DNA repair enzyme,
What’s often overlooked are the factors that’s driving the DNA errors that transform the breast cell into cancer cells in the first place.
So although I inherited a faulty BRCA-1 gene that’s been associated with a high lifetime risk of breast cancer (~80%), when I was diagnosed, I had no family history of breast cancer.
How can this be when I have a huge family?
Remember that BRCA-1 is a DNA repair enzyme and having a faulty BRCA-1 gene isn’t the proximal cause of breast cancer.
There had to be something in the first place that resulted in DNA damage in one of my original breast cells that finally grew into a tumour in my left breast.
You see, my family migrated to Australia from Indonesia when I was six years old.
So if you compared how I lived and how my relatives lived, there are vast differences in the physical, behavioural and social risk factors for breast cancer.
So could there be factors protecting my female relatives living abroad from breast cancer?
Maybe.
Or has my breast cancer risk factor profile increased dramatically because I grew up and lived here in Australia for many years- and have adopted a more “high-risk” lifestyle?
Most likely.
From migration studies, we can see that the risk of breast cancer in Japanese women living in Hawaii is far higher than that of a Japanese woman in Japan.
Their genetics are the same but because they’ve migrated, their environment has changed.
Prevention isn’t a Dirty Word.
So after much reading and research, one thing is for sure.
There is NO UNIVERSAL CAUSE of breast cancer.
Can you imagine being a scientist and trying to study ONE woman’s genetic, lifestyle and environmental risk of breast cancer. The interplay of risk factors and protective factors could possibly be additive, multiplicative or subtractive.
There would be a dizzying amount of variables to measure and control for.
In other words, each woman’s breast cancer causation profile is going to be a set of genetics, lifestyle and environment factors that is unique to her.
So let’s throw out the notion that any researcher would or could ever study our lives in great detail.
Can we figure out our own risk profile?
I believe we can and we should.
I think the first step is to have a little COURAGE to WANT to understand.
It’s easier to bury our heads in the sand because it’s too scary to really figure this all out.
It’s easier to live a lifestyle and environment that we are use to and comfortable with.
BUT if we’re open to change…
…I believe that those who have had a diagnosis of breast cancer can take reasonable steps to modify their lifestyle and environment so as to prevent a recurrence.
And those that have a strong family history of breast cancer can become more aware and educated as to the cause of breast cancer and feel empowered to prevent breast cancer from ever developing.
Suggested Further Reading:
My Top 10 Evidence-Based Anticancer Supplements
If you've been diagnosed with cancer and looking to take supplements to bolster your anticancer defences then this article is a must read! These top 10 science-backed supplements not only protects you against cancer, they also protect you from the harsh side-effects of cancer treatment
This post may contain affiliate links. Please read our disclosure for more info.
I ignored my doctor.
Two years before my cancer diagnosis, my vitamin D levels came back dangerously low.
My doctor said, "You need to supplement."
I said, "I don't like swallowing pills."
And I did nothing.
Two years later, I was sitting in an oncologist's office being told I had Stage 2B triple negative breast cancer.
I was 29 years old.
And one of the first questions I asked myself was: Could I have prevented this?
I'll never know if low vitamin D contributed to my cancer. The research suggests it might have. But what I DO know is this:
I wasn't going to make that mistake again.
The moment I was diagnosed, I became obsessed with one question:
What can I DO—right now, today—to give my body every possible advantage in this fight?
Chemotherapy would attack the cancer. Surgery would remove it. Radiation would kill any remaining cells.
But what could I do to support my body THROUGH that treatment? To reduce side effects? To lower my risk of recurrence?
That's when I started researching supplements.
And let me tell you—it was overwhelming.
There are thousands of supplements marketed to cancer patients. Naturopaths recommend one thing. Integrative oncologists recommend another. Facebook groups swear by protocols that cost $500 a month.
I didn't know what actually worked. What was evidence-based versus expensive snake oil. What was safe during chemo versus what could interfere with treatment.
So I did what any terrified scientist would do:
I read every study I could find. I consulted with a naturopath and later an integrative medicine doctor. I experimented (carefully, with my oncologist's approval).
And over 15 years, I figured out what actually matters.
Today, I'm going to share exactly what I took during treatment—and what I take now to stay cancer-free.
But first, let me be crystal clear about something.
This is not medical advice.
I'm a PhD biochemist and a 15-year breast cancer survivor, but I'm not YOUR doctor. What worked for me might not work for you. What was safe for my treatment protocol might not be safe for yours.
You MUST talk to your oncologist before taking ANY supplements during active treatment.
I know some oncologists are dismissive about supplements. I know some will say "those don't do anything" or "just eat a balanced diet."
But you still need to tell them what you're taking.
Why?
Because some supplements can interfere with treatment. Some increase bleeding risk (dangerous before surgery). Some reduce the effectiveness of chemotherapy or radiation.
My oncologist gave me the okay to take supplements during treatment—but with strict rules:
Stop 3 days before chemo
Stop 3 days after chemo
Only take on non-radiation days during radiation therapy
Your oncologist might have different guidelines. Or they might say no supplements at all during active treatment.
You have to honor that.
I'm sharing my personal supplement protocol for three reasons:
1. Because I wish someone had given me this roadmap when I was diagnosed.
I wasted so much time and money trying to figure out what mattered. I want to save you that.
2. Because I want you to understand my THINKING—not just copy my list.
Your goals might be different than mine. Your cancer might be different. Your budget might be different.
I'm going to show you how I prioritized so you can make informed decisions for YOUR situation.
3. Because partnering with a professional is worth it—but not everyone has access.
I worked with a naturopath and later an integrative medicine doctor. It was expensive, but it helped me avoid the "shotgun approach" of taking 47 different supplements with no strategy.
If you CAN work with an integrative oncologist or naturopath, do it. They can tailor a protocol to YOUR cancer, YOUR treatment, YOUR goals.
If you can't, this guide will help you prioritize.
MY SUPPLEMENT PHILOSOPHY (The Framework):
Here's how I think about supplements:
Not as a replacement for treatment. As strategic support.
I wasn't trying to "cure cancer with vitamins." I was trying to:
✓ Give my body the best possible foundation to tolerate aggressive treatment
✓ Reduce short-term side effects (neuropathy, fatigue, nausea)
✓ Prevent long-term damage (heart toxicity, bone loss, cognitive decline)
✓ Lower my risk of recurrence after treatment ended
Different phases require different supplements.
What I took during chemo was different from what I took during radiation. And both were different from what I take now in long-term survivorship.
Quality matters more than quantity.
I'd rather take 3 high-quality, evidence-based supplements than 20 cheap ones with questionable bioavailability.
Good supplements aren't cheap. But they're cheaper than taking things that don't work.
Evidence matters.
I'm a scientist. I wanted supplements with actual research behind them—not just testimonials from wellness influencers.
That doesn't mean "FDA-approved" (supplements aren't regulated that way). It means: Are there peer-reviewed studies showing this compound has anticancer activity? Is it bioavailable in the form I'm taking? Is it safe during treatment?
MY SUPPLEMENT PROTOCOL (Organized by Phase):
PHASE 1: THE ESSENTIALS (What I Take Every Single Day—Then and Now)
These are the non-negotiables. The ones with the strongest evidence for anticancer activity and the best safety profile during treatment.
1. Essential Supplements
Vitamin D3 5000IU/day
"In studies of cancer cells and of tumors in mice, vitamin D has been found to have several activities that might slow or prevent the development of cancer, including promoting cellular differentiation, decreasing cancer cell growth, stimulating cell death (apoptosis), and reducing tumor blood vessel formation (angiogenesis)" - Cancer.Gov
Vitamin D is involved in hundreds of biological processes—immune function, cell differentiation, apoptosis (programmed cell death of cancer cells), and angiogenesis prevention (stopping tumors from forming blood vessels).
The research is clear: Low vitamin D levels are associated with higher breast cancer risk and worse outcomes.
In fact, many women with breast cancer (including me) had low vitamin D levels before diagnosis.
After I was diagnosed, I got my levels tested. They were still low.
I immediately started supplementing—and I've taken vitamin D3 every single day for 15 years.
What to look for:
Most vitamin D supplements at the drugstore are weak (100-1,000 IU) and come in giant capsules.
I use Healthy Origins Vitamin D3 (5,000-10,000 IU in a tiny gel capsule). It's highly concentrated, easy to swallow, and cheap.
During treatment: My oncologist approved this throughout chemo and radiation.
Now: I take 5,000 IU daily and get my levels tested annually to make sure I'm in the optimal range (50-80 ng/mL). Most vitamin D3 you'll find at the chemist comes in a weak formulation (usually 100IU) and comes in big capsules. I really love the Healthy Origins brand because they come in a tiny concentrated gel capsule (you can get up to 10,000IU). They are easy to swallow and it's super cheap!
Favourite Vitamin D3:
Curcumin
Curcumin is the active compound in turmeric—and it's probably the most researched anticancer supplement on the planet.
It has broad-spectrum anticancer activity, meaning it works against multiple cancer pathways:
Inhibits cancer cell growth
Triggers apoptosis (cancer cell death)
Reduces inflammation
Prevents metastasis
Blocks angiogenesis
There are literally thousands of studies on curcumin and cancer. Here's a review specific to breast cancer.
The problem: On its own, curcumin is poorly absorbed by the body.
You can eat turmeric in your food, but you won't get therapeutic doses that way.
The solution: You need a bioavailable form—one that's been formulated to actually absorb.
I take Life Extension Super Bio-Curcumin because it uses BCM-95, a patented form that's been shown in studies to be 7x more bioavailable than standard curcumin.
During treatment: I took this throughout chemo and radiation (on non-treatment days) with my oncologist's approval. Curcumin is the active anticancer compound derived from the root plant turmeric and is probably the most studied anticancer compound to date. You can read a scientific review on curcumin and breast cancer here.
Due to the overwhelming evidence of curcumin and its anticancer properties, it's no surprise that I've added curcumin in my essential supplements list.
A word of caution - on its own, curcumin is difficult for the body to absorb so it's important to take a good quality and bioavailable form. The Super Biocurcumin from Life Extension is excellent quality and one that I’ve personally been taking twice daily since I was first diagnosed until today.
Favourite Curcumin:
Why I took it during treatment:
High-quality fish oil reduces inflammation, supports heart health (critical during chemo—some drugs are cardiotoxic), and may improve treatment outcomes.
Some studies suggest omega-3s help reduce chemotherapy-induced neuropathy and support cognitive function (aka "chemo brain").
What to look for:
NOT all fish oils are created equal.
You want:
High concentration of EPA/DHA (not just "1000mg of fish oil"—that's mostly filler)
Third-party tested for purity (no mercury, PCBs)
Triglyceride form (better absorption than ethyl ester)
I used Nordic Naturals Ultimate Omega or Life Extension Super Omega-3.
During treatment: 2-3g daily (split into 2 doses with meals).
Now: I still take 2g daily. Another tip is to get an enteric coated fish oil. It's slightly more expensive but it's worth it if you're experiencing reflux symptoms.
Favourite Omega 3:
2) Supplements I Took During Treatment
MGN-3 probably one of the most expensive supplements I took and one that my naturopath prescribed me. From what I've researched, MGN-3 increases the activity of your natural killer cells. It is developed and manufactured in Japan by Daiwa Pharmaceutical Co, Ltd, and marketed worldwide as a nontoxic food supplement under different brand names such as BioBran (Globally), Lentin Plus (Japan/Asia), Ribraxx (Australia/New Zealand), BRM4 (United States). You can check out studies of MGN-3 for yourself here. In Australia, we can order Ribraxx through a health practitioner.
One of the most important things you can do during cancer treatment is to not become immunodeficient. Not only to avoid infections, but also to still be able to fight cancer when treatment has finished.
Maitake mushroom is an edible fungus that is popularly consumed in Asia especially Japan. It has gained popularity as a supplement because of it's ability to stimulate the immune system. The D-fraction from edible and medicinal mushrooms have been shown to show antitumoral and anti-metastatic activities in triple negative breast cancer. You can read the study here.
Favourite Maitake supplement:
Why I took it during treatment:
Some chemotherapy drugs (like Adriamycin) are cardiotoxic—they can damage your heart.
CoQ10 supports mitochondrial function and protects the heart.
There's also some evidence it may reduce chemotherapy-induced fatigue.
What to look for:
Ubiquinol form (more bioavailable than ubiquinone, especially for cancer patients whose bodies are stressed).
I used Qunol Ubiquinol or Life Extension Super Ubiquinol CoQ10.
During treatment: 100-200mg daily (I discussed this with my oncologist first—some are cautious about antioxidants during chemo, though CoQ10 is generally considered safe).
Now: I take it a few times a week for heart health and energy.
You can read about studies of CoQ10 and the impact it has on maintaining cardiovascular health here.
Favourite CoQ10:
Green tea catechins (especially EGCG) have strong anticancer properties and may reduce recurrence risk.
I didn't take this during active treatment because there's some debate about high-dose antioxidants during chemo/radiation.
But post-treatment? It's one of my staples.
What to look for:
Decaffeinated (unless you want the caffeine).
Standardized to at least 45% EGCG. In animal studies EGCG has been shown to block angiogenesis -the process by which tumours establish a new blood supply - critical for cancers to grow and spread.
In another study it's been shown that daily consumption of green tea results in a lower breast density compared to non-tea drinkers. We know that increased breast density is a risk factor for breast cancer. However, this effect was mainly seen in post-menopausal women. You can read the scientific reviews of green tea and its effects on breast cancer here.
I drink several cups of green tea (~6 cups is beneficial) per day and take green tea supplements to further increase the levels of EGCG in my body.
Supplements I Take Now
We all know that vitamin C is really good for our immune system, however, it's been shown that high doses of vitamin C can directly kill cancer cells which you can only achieve intravenously.
After consulting with my IMD at the National Institute of Integrative Medicine, I underwent a year of fortnightly intravenous vitamin C (every 2-3 weeks). After that initial year I just supplemented with vitamin C tablets.
Favourite Vitamin C:
Modified citrus pectin (MCP) is derived from the rind and of citrus fruits. It needs to be modified for us to able to absorb it in the gut. MCP can affect the different steps in cancer metastasis. You can read a review of MCP here. MCP is a also a good detoxifying supplement to take as it has been shown to chelate heavy metals in your body and removing them via the urine.
Diindolemethane (DIM) are metabolites derived from cruciferous vegetables such as broccoli and brussel sprouts. It helps your liver metabolise toxic oestrogen. Therefore it may be especially beneficial for those of you with oestrogen positive breast cancer as it can lower your oestrogen levels rather than just blocking oestrogen receptors (the way that tamoxifen works).
So if for some reason you can't take tamoxifen, then taking estrodim could be a viable alternative.
Studies have shown it can also benefit hormone negative breast cancer patients as it has anticancer properties beyond oestrogen metabolism. For example, it can restore p21 gene activity and stops tumours from developing a blood supply. You can read on the scientific review of DIM here.
Favourite DIM supplements:
This is by no means an exhaustive list of anticancer supplements. There's many more that I take but from my research these ones seem to have the most scientific evidence for it's anticancer properties.
f I could go back to 2010 and give myself a supplement protocol, here's what I'd say:
START HERE (The Bare Minimum):
Vitamin D3 (5,000 IU)
Curcumin (bioavailable form)
Omega-3s (high-quality fish oil)
That's it. Those three.
If you can only afford three supplements, those are the ones with the strongest evidence and the best safety profile during treatment.
THEN, if you have the budget and your oncologist approves:
Probiotics (for gut health during chemo)
CoQ10 (for heart protection)
L-glutamine (for neuropathy prevention)
POST-TREATMENT, add:
Green tea extract
Medicinal mushrooms
DIM (if relevant to your cancer type)
WHAT I WISH I'D KNOWN:
You don't need to take everything.
I wasted money on supplements that didn't have strong evidence or that I couldn't tolerate.
Focus on the essentials. Do them well. Don't try to do everything.
Quality over quantity.
Three high-quality supplements beat 20 cheap ones.
Timing matters.
What's safe during treatment might be different from what's optimal post-treatment.
Your oncologist might not know about supplements—and that's okay.
Most oncologists aren't trained in integrative medicine. If they dismiss supplements entirely, consider getting a second opinion from an integrative oncologist or working with a naturopath in addition to your oncology team.
You are allowed to be proactive.
Taking supplements doesn't mean you're chasing false hope or falling for pseudoscience.
It means you're doing everything you can—with the best evidence available—to give your body every advantage.
And 15 years later, I'm still here.
Still taking my vitamins.
Still cancer-free.
5 Great Stories of Long Term Triple Negative Breast Cancer Survivors
For 7 years, knowing there were long term survivors for TNBC was one of the key things that kept me positive. It was the one fact that I could cling to that kept me going when things were tough. You see, when I got that diagnosis I knew it was serious. The emotions I felt during those first few weeks were the darkest I've ever felt in my life.A part of me believed it was a death sentence, but the survival part of me began searching for real-life proof that it wasn't so. Even though I'm a scientist by training, I didn't want statistics. I needed a more human kind of proof.
You’ll have to agree with me that when diagnosed with a serious illness like breast cancer, you need a positive attitude to get through it.
It's a huge struggle getting through breast cancer treatment, and for many women that challenge extends beyond the physical. The sheer amount of mental hurdles that we face can drag us down at any stage of the journey.
So when you've just been diagnosed, how do you remain optimistic when faced with having an aggressive type of breast cancer - Triple Negative Breast Cancer.
For 7 years, knowing there were long term survivors for TNBC was one of the key things that kept me positive. It was the one fact that I could cling to that kept me going when things were tough.
You see, when I got that diagnosis I knew it was serious.
The emotions I felt during those first few weeks were the darkest I've ever felt in my life.
A part of me believed it was a death sentence, but the survival part of me began searching for real-life proof that it wasn't so.
Even though I'm a scientist by training, I didn't want statistics. I needed a more human kind of proof.
So I searched google and found an Australian breast cancer forum (this was before the advent of facebook groups)
I quickly signed up and in the forum I called out...
"Are there any long term triple negative breast cancer survivors out there???"
But no one responded.
So I thought to myself:
"Does that mean none of them survived?"
Finally, after a couple of weeks someone chimed in and mentioned there was a 15 year TNBC survivor - but she wasn't active in the forum anymore.
That was my "AHA" moment. The lightbulb switched on in my head.
Well of course no long term survivors were gonna be in the forums - they had gotten on with their lives!
Even though I didn't manage to contact that particular survivor, and I didn't know her name and had never seen her face, knowing she was alive helped me immensely. Because I knew that if she could do it, then I can too!
That mindset switch ... was POWERFUL.
From thinking this was going to be a death sentence to finally seeing a glimmer of hope that I can survive this, was one of the fundamental things that saved me from despair.
Fast forward 7 years later, I am a long term survivor.
I knew that I wanted to share the same inspiration with women who are newly diagnosed and those who are afraid.
Today, I want to share my story and five other stories from women who are long term triple negative breast cancer survivors.
All of us are alive and well. Some of the women have just passed their 5 year mark, whilst others are approaching their 10th year as a survivor.
They've also kindly and selflessly shared their words of wisdom along with their pathology, treatment regimes and outcome. Even though every woman's journey is different and unique, there are some things that we as survivors all share.
There are some truths that we can all relate to.
So, let's start with my story...
My journey with breast cancer started when I felt a huge lump on my breast when I was showering one night. I went to the doctor and the next day my general practitioner felt the lump and told me not to panic as it was probably just a benign lump and lots of young women had it. I wanted a mammogram to confirm and I didn't take no for an answer. This was probably the first time that I found my voice and understood the importance of being my own advocate.
I happily drove to the imaging clinic and again I was reassured there was nothing to worry about (because I was young) and all I needed was an ultrasound - no mammogram. So after the ultrasound was complete, and they told me I had to stay back for a mammogram - I knew I was in for some shattering news.
I was diagnosed with TNBC in September 2010 with a 2cm lump shown on mammogram and scans showed an enlarged lymph node in my armpit. I underwent neoadjuvant chemotherapy consisting of 6 rounds of 3-weekly Docetaxel, Doxorubicin and Cyclophosphamide (TAC).
My lump had noticeably shrunk after the first round of chemo and by the 6th round, I couldn't feel anything.
I was relieved my treatment was working.
I had a single mastectomy and pathology tests of the breast tissue and lymph nodes showed a complete pathological response to the chemotherapy. There were no cancer cells left.
I was also given a choice to have radiation and decided to go for it. I had a prophylactic mastectomy on my other breast during reconstruction because I tested positive for the BRCA1 mutation.
Truth #1: No matter what, when receiving your diagnosis, you'll feel blindsided.
So when I was diagnosed, I was happily planning my wedding.
No matter who you talk to - their breast cancer diagnosis always came at the worst possible time.
What was supposed to be a happy time in my life became a nightmare. Instead of trying on wedding dresses, my life suddenly revolved around doctor's appointments, scans, multiple hospital visits and people praying for me.
I mean who at 29 think they're about to get diagnosed with cancer? Cancer wasn't even on my radar.
This was also true for Hilary DeMitry-Perez (5 year survivor) who had just given birth to her second son a month before her diagnosis in February 2013.
She was having difficulty breastfeeding her baby when she noticed a lump. Initially her doctor thought it was a blocked milk duct, but since it didn't aspirate easily, her doctor sent a sample to be biopsied.
Unfortunately, her results came back and she was diagnosed with Stage 2 TNBC. She had a lumpectomy followed by chemotherapy which consisted of AC followed by dose-dense Docetaxel and radiation.
Hilary has no family history of breast cancer and is BRCA negative.
"There are many long term survivors who are doing well after cancer treatment. We're not always active in support groups because we're out living our life."
It's not easy getting through cancer treatment, and it's even more challenging when you have little ones to take care of. Here are Hilary's tips for managing treatment and taking care of young kids...
"Ask for help when needed. Be specific about asking what you need as often there are people who want to help but don't know what's needed. Also, manage your own expectations - it's ok to order pizza or dinner out, it's ok for the kids to watch TV if you're tired, it's ok to let the housework go until you have more energy. Do what you need to take care of yourself."
Today Hilary spends as much time as possible with her husband and two boys age 5 and 10. She works full time as a social worker and travels as much as possible. She loves going to see live music, theatre and playing Texas Hold Em Poker. She was just chosen to walk in the Survivors Parade at Churchville Downs in Louisville, Kentucky.
Hilary's words of wisdom...
"Living life is essential - spend time with supportive friends and family, engage in the activities you enjoy and do something you've always wanted to do. And don't be afraid to ask for help if you need it including seeking out mental health or spiritual counselling."
Truth #2: There's going to be speedbumps along the way - anticipate the setbacks.
Scherri Woodard was diagnosed with Stage 3 TNBC in March 2009 at the age of 43 after finding a lump in her right armpit during a breast self-exam.
Scherri had a previous history of cysts so her doctor wasn't too worried about the lump, until it grew to the size of a golf ball.
Her surgeon tried to drain the cyst, and when that was unsuccessful, they sent some samples to be tested. She was diagnosed with TNBC a few days later.
For her treatment, Scherri underwent neoadjuvant chemotherapy which consisted of 4 rounds of AC and 4 rounds of Docetaxel.
She had a double mastectomy despite testing negative for any BRCA1 or BRCA2 mutations.
Her pathology came back positive for residual disease in 9 out of 26 lymph nodes. Her breast tissue was clear.
When I asked Scherri how she felt getting the results of her pathology after surgery, she said:
"I wasn't too worried since I knew I was going to do radiation. I guess I just had faith that I was in good hands and would be okay."
As Scherri approaches her 10th year since her diagnosis, she has this to say to those just starting their treatment.
"Celebrate even the smallest of milestones like when you're halfway through chemo or a quarter of your radiation treatments. Go do something for yourself. It doesn't have to be much just do something for YOU!"
"I got through the tough times by laughter... lots of laughter. I have a very strange sense of humour and that is the one thing that I could count on to get me through the worst of it."
I couldn't agree more with Scherri!
My fiancé at the time (now my husband) always tried to make me laugh the whole time I was going through treatment. He made me promise to him in the beginning that I was going to be a "happy cancer patient". It's true what they say that the journey is just as important as the destination. Breast cancer is a serious disease, and we can't predict what the future holds for us, but if we can still bring joy and laughter at even the most stressful of times, we can be more resilient than ever.
Jade Richards also had some setbacks during treatment but she was able to remain optimistic through out. She was 33 when she was diagnosed in February 2012.
Her tumour measured 2.8cm and was positioned up high on her breast. She opted for a lumpectomy, however it turned out the surgeon didn't get clear margins and the pathology showed 2 out of the 4 nodes were positive for cancer. Her medical team went in for another round of surgery, but the second attempt to get clear margins also failed.
The two failed attempts was due to the cancer growing so quickly so her doctors decided on chemotherapy right away. After chemo (FEC + Docetaxel) Jade underwent a single mastectomy and radiotherapy. She also had a DIEP reconstruction and reduced the size of her contralateral breast.
It was only last January that Jade found out she was positive for the BRCA1 mutation. She recently had a prophylactic salpingo-oophorectomy (removal of ovaries and uterus) and will soon have a preventative mastectomy on her other breast.
Even though Jade was diagnosed with TNBC as a young woman she was never offered genetic testing by her doctors prior or during her treatment.
"I wasn't aware if I was tested or not. I asked my consultant and he said I never had the test. I'm so upset because all the reconstruction I had is now ruined, I could have had the surgery all at once. I’m just glad it never returned after all these years, as I feel like a sitting duck..."
Jade is thankful to still be NED (No Evidence of Disease) after 6 years and she has a message for those who are newly diagnosed with TNBC.
"Try to remain calm. Your diagnosis doesn't mean the worst so take time to digest what you're told. Buy a notebook and write down every single question you have. Write down the things you want or need to do. Find support, and if there isn't one you're not alone - try online support groups. They're amazing and understand your situation. Remember, we got through this and you will too!"
This leads us to our third truth.
Truth #3: Trust your intuition - be your own advocate.
I can totally relate to Jade's missed genetic testing during her diagnosis.
After the initial shock of finding out I had breast cancer, I brought up genetic testing with my own oncologist. He dismissed me and instead urged me to concentrate on the diagnosis at hand, and there'll be plenty of time to research the genetics side of things afterwards.
What he told me made perfect sense and even my breast surgeon said the same thing, but my gut was telling me to dig deeper.
I'm grateful that I trusted my intuition and sought advice from my general practitioner who helped me get a second opinion.
That second opinion saved me from having multiple surgeries.
You see, I tested positive for BRCA1+ despite being of Asian heritage and having no family history of breast cancer. The outcome of my genetic testing resulted in my surgical recommendation changing from a lumpectomy + radiation, to mastectomy + radiation.
What I often hear people say, is that you have to completely trust your medical team.
But the truth is, the process of diagnosis and treatment is complicated. It's handled by a multidisciplinary team - consisting of many physicians, technicians and nurses, each responsible for their field of specialty.
It's not a perfect process.
Your job is not just to be a good patient and follow "doctor's orders". You need to be a proactive patient.
Think of your medical team as your trusted advisors. But ultimately if your gut says that something isn't right with the advice, to speak up and be heard. Getting a second opinion doesn't mean that you need to switch doctors. It just means you're doing your due diligence.
So the important point to remember is to::
Ensure you have all the information you need to make a decision
Be thorough and ensure nothing is amiss from the point of diagnosis, treatment and follow up
Don't be intimidated by your doctor, feel silly, or awkward. Ask all the questions you need.
Remember, the devil is in the details.
Truth #4: We all fear a recurrence - but the feeling gets less intense with time
When treatment was over I booked a major holiday for myself and my hubby - a well deserved trip to New York City (I live in Australia so it was a big trip for us!). During the last half of the trip my ribs started hurting badly. I was devastated and hysterical fearing the cancer had come back. Luckily the bone scan showed nothing and I was still NED.
After a couple of episodes of false alarms, I began trusting that my body was ok. It took a while for me but as time went on, I was gaining more and more confidence in planning out my life.
Marilyn Buchheit is approaching her 9th year as a TNBC survivor. She was 65 when she was diagnosed with Stage 3 TNBC in 2009.
"I do believe every survivor gets scared about this. Every year that goes by, my thoughts about a recurrence does diminish, but when you get a pain somewhere, the thought of cancer is in the forefront of my mind."
Marilyn opted for a double mastectomy with no reconstruction and the pathology revealed a 5.5cm tumour in her breast along with 1 lymph node involvement. She had adjuvant chemotherapy involving Doxorubicin, Cyclophosphamide (AC) and Paclitaxel (Taxol). She was also given an angiogenesis inhibitor Bevacizumab (Avastatin) and 6 weeks of radiation therapy. Marilyn is positive for the BRCA2 mutation.
Marilyn's words of encouragement...
"Take the time to cry and feel sorry for yourself. Then get up and start fighting for your life, rather than to worry. God has a plan for each and every one of us."
Truth #5: We do it for our family
I didn't have kids when I was diagnosed. And I share those same feelings of dread about chemotherapy affecting our fertility.
It's like we'll be damned if we do and damned if we don't.
I was fortunate to have a round of of IVF before chemo but I had a rare complication called ovarian hyperstimulation syndrome and was hospitalised because my kidneys had shut down.
Fluid had built up in my tissues and lungs and I wasn't able to breathe properly. I couldn't have been in the worst situation because now my treatment was delayed.
I'm glad to say there was a happy ending - I was able to conceive naturally five years after my treatment had finished and it only took one month of trying.
As a mum, our biggest fear is to leave our kids without a mother. With many TNBC patients being young women with young families, it's even more painful when you think you could be missing out on seeing your kids grow up. Our next survivor is Tammy Willmore and her story inspires us to keep fighting on so we can see our kid's achieve great things and experience their major milestones in life.
"My daughter was 11 years old when I was diagnosed and I thought I'd never get to see the day of her wedding. "
Tammy discovered a lump on her left breast after her Labrador retriever jumped on her chest. After a couple of days of burning pain she had a mammogram and a few days after her biopsy, she was diagnosed with a 2.5 cm tumour, Grade 3, Stage 2b in May 2008. She started her treatment with neoadjuvant chemotherapy which consisted of 3 rounds of FEC (5-FU, Epirubicin and Cytoxan) and 3 rounds of Docetaxel (Taxotere).
She felt the tumour shrinking right away and by the end of chemo, she couldn't feel the lump at all. She had a lumpectomy and lymph node dissection which confirmed a complete pathological response. She also had 35 radiation treatments on the recommendation of her doctors. Tammy has no family history of cancer and is BRCA-negative.
Tammy's words of wisdom....
"Live life to the fullest and make memories. I was such a perfectionist before cancer that I was always so stressed because of course no one can achieve perfection. I never did anything spontaneous. I didn't know how to live in the moment - cancer changed all that! I took a trip to Florida by myself this winter and had an awesome time! I'm going to Cancun Mexico on a spur of the moment trip with my daughters. So live in the moment! My messy house will be there when I get home!"
Truth #6: Healing isn't over when treatment is done.
After cancer treatment, we often feel worse off than when we started.
To this day Tammy still battles with side-effects from cancer treatment. She has lymphedema in her left arm that's managed with physical therapy and compression sleeves. She was also diagnosed with osteoporosis a year ago due to early-onset menopause caused by the chemotherapy.
Tammy says:
"I have days that I feel 20 years older - low energy, arthritis but I try not to give in to it. I ride horses, hike, and I kayak when the weather is warm."
For me personally, I've been fortunate enough to not have any long-term physical side-effects. It's easy to slip back into "business as usual" after treatment ends. But we need to find that delicate balance between living life to the fullest and being vigilant about our health.
Since day 1 of my diagnosis, I've made a deeper commitment to my health. Having a diagnosis of breast cancer woke me up to the fact that I needed to invest more time and resources into my health. I know that true health can give us the freedom that we desire in our lives.
I wasn't going to survive breast cancer and be diagnosed with some other disease at a later stage. And if the time comes that I did have a recurrence, I would be in the best shape of my life to withstand another round of treatment.
I prioritise my health above all else.
Even my family.
Because I know that the stronger I am, the stronger they will be.
I hope you enjoyed reading our stories.
Although every woman's diagnosis and journey is different, there are some things that we all share.
When faced with breast cancer, we share the same emotions, worries and hopes for the future. It's what ultimately make us human.
Trifina Sofian is a coach specializing in cancer recovery and mindset management. She empowers cancer survivors to master their mental state, beat cancer, and unlock their body's full healing potential. Trifina will reprogram your mind to conquer cancer and transform your state of mind and body.
Get her powerful new book Win the Fight Against Cancer - How to Master the Mental Battle HERE and start your transformation today.
I Had These 5 Signs & Symptoms of Breast Cancer (Plus How I Avoided a Misdiagnosis)
Do you have these 5 signs and symptoms of breast cancer? I suffered these symptoms years before I could feel a lump and was diagnosed by my doctor. I was only 29 years old when I was diagnosed with no family history of breast cancer so this was such a scary thing for me. My doctor wasn't worried and dismissed it. In this post I want to share with you these signs and symptoms in the hope that I can save one woman's life by diagnosing at the early stages and not letting anyone ignore her concern.
**This post is for informational purposes only and is not intended as medical advice. Please see a qualified health professional if you have any concerns.
There’s lots of awareness about the importance of self breast exams and getting the doctor to examine your breasts. But did you know some women with breast cancer can't feel a lump and there are other symptoms of breast cancer that could show up even earlier?
In my case, one of the symptoms I had popped up YEARS before I noticed the lump.
I’m kicking myself, because I should have taken notice of those early warning signs, but instead I ignored them, and hoped they would go away.
Imagine if I did investigated further, could I have avoided chemo, a mastectomy and radiation?
It’s important to remember that detecting breast cancer in its early stages is favourable because the prognosis is so much better for these women. I'm hoping by writing this post, I can give hindsight to another person. Remember, men can get breast cancer too! (although it's rare).
So let’s get right into it and let me describe the symptoms I had prior to my breast cancer diagnosis.
1| Swelling under the armpit
This was probably the earliest symptom of breast cancer that I had going back a couple of years from diagnosis. The closest lymph nodes to the breasts are the ones on your underarm and collarbone. So any stray cancer cells would drain to these lymph nodes first.
I was having a massage when the therapist commented that she could feel something under my armpit. I honestly couldn't feel much discomfort until she pressed quite hard it did become tender. She told me to go check it out but unfortunately I didn’t really pay much attention at the time and shrugged it off as nothing.
Because a massage therapist uses alot of pressure when they’re massaging, they can get real deep into the tissues and feel for any lumps or swelling that you yourself don't normal feel. I've personally heard stories of women finding out lumps on their breasts when they’re having a massage, so next time the massage therapist kindly tells you there’s a lump, do yourself a favour and see a doctor.
You could be fighting an infection of some kind which may explain the swelling of the lymph nodes, but at least by seeing a doctor, they can monitor the swelling.
2| Fatigue
I had been pretty tired for a couple of years before I was diagnosed. I suspected I was low in iron but the iron supplements weren’t helping. I also tried exercising to boost my energy levels, so I joined the gym and got myself a personal trainer. Usually most people will get a endorphin high after a workout but the opposite happened. I felt like my head was pounding and I wanted to slip into a coma.
Tiredness is a pretty general symptom to have so it’s somewhat difficult to know if something sinister is going on.
The tiredness I felt was even more pronounced in the couple of months leading to the diagnosis.
To clarify, it was more than just feeling tired, I was fatigued. I felt like I needed a nap after I just had one.
3| Changes to the Nipple
Nipple-related changes usually occur on the side where the breast cancer is growing. This was probably one of the biggest clues that I totally ignored (stupid me!) and there were several nipple-related changes that I want to mention.
Firstly, I had itchy and cracked nipples. This went on and off for a couple of months. It wasn’t constant and I suspected I might have been allergic to a new soap or a new bra that I got. Because I also started exercising, I put it down to lots of sweating and rubbing being the cause. My nipple also soon became inflamed, scaly and peeling.
I also experienced a clear and sometimes milky discharge when the nipple was squeezed (I wasn’t pregnant or breast-feeding at the time). Some women notice a bloody discharge.
Other nipple related changes that some women have reported include nipple retraction (turning inwards), flattened nipple, a rash or decrease in sensitivity.
4) Night sweats
I experienced night sweats 2-3 times prior to diagnosis which I had mistakenly thought was overheating because I had too much doona while sleeping. I would wake up in the middle of the night with a drenched pyjama top. Scientists don’t really know what causes night sweats in cancer but my guess would be the body’s immune system trying to mount an attack or some type of hormone changes caused by the breast tumor itself.
5| Breast Lump
When I was diagnosed, I couldn’t believe how big the tumor was already.
How could I not have noticed it earlier? It felt like a huge lump appeared out of nowhere.
The breast surgeon explained to me that in order to feel the lump, it had to have a different density to the surrounding breast tissue. So in my case when the tumour was smaller it wasn’t dense enough to be felt. Because I was in my 20s, I wasn’t even doing breast exams, so it was very possible that it was there and I just never felt it until it got very big.
So those were my symptoms. Other possible symptoms of breast cancer can also include:
Skin irritation or dimpling
Swelling of all or part of the breast (even if no distinct lump is present)
Upper back, shoulder and neck pain
Pain in the breast or chest
This isn’t meant to be an exhaustive list of symptoms and each women will present differently or not at all until they are in a screening program, so it’s important to know what’s normal for your breasts.
If you notice anything out of the ordinary or abnormal about your breasts, then it’s a good idea to get it checked out by a doctor. It might be nothing serious, and worst case scenario it was a false alarm.
A Near Misdiagnosis
When I did eventually find the lump in my breast, I went to see the doctor straight away. But would you believe it, she didn’t even think it was breast cancer and was about to send me on my way!
When my doctor, an elderly woman, examined my breasts, she assured me there was nothing to worry about and it’s probably a fibroadenoma - a benign cyst. She saw it all the time in young women (basically she was saying she had X number of years experience and that I should trust her on this one).
Her advice was a wait and see approach and told me to come back in a couple of months.
At this point I was in a panic that she didn’t believe anything was wrong. Sure she examined my breasts, but she didn’t have x-ray vision, how did she know it wasn’t breast cancer?
So of course I put on the waterworks and basically told her I wouldn’t be able to sleep at night until I get a proper scan (I had an ultrasound and mammogram that same afternoon).
Now don’t let any doctor, intimidate you or feel like you’re a hypochondriac. If they do then perhaps it’s time to change doctors.
But imagine if I did took her advice and waited two or three whole months?
Could my diagnosis be different? Would I have been a Stage IV cancer patient with metastatic breast cancer?
Would I even still be alive today?
Who knows.
I honestly don’t blame the doctor. Doctors are humans after all and they make assumptions about us. She took one look at me - a young woman presenting with a breast lump, and assumed the chances of breast cancer was pretty low so in her mind, there was no reason to investigate further.
The important thing to learn here was that I got to the bottom of it and not shrugged it off - like I did with all the other signs and symptoms of breast cancer.
Did you find this post useful? If so don't forget to share it!
Getting Back to Healthy Eating + Helpful Tips for the Busy Person
When I was first diagnosed with cancer, it was a huge wake up call for me to evaluate my lifestyle and made me aware of how unhealthy I was living. Because I was so scared that cancer would get the best of me, I was hugely motivated and changed my eating habits instantly.
I would juice a few times a day, eat all the cruciferous vegetables, minimised my meat consumption and avoided dairy and sugar. It was easy peasy because at that point in my life, fear was driving me to eat healthy in a way I had never done before.
However, it’s now been six years from diagnosis. The anxiety and fear of a cancer recurrence has somewhat dissipated and frankly so has my motivation for healthy eating.
My life also looks different now. Busier. (Who's life isn't?).
I'm now focused on caring for my daughter. And it's hard work, taking up all my time and energy.
I've finally managed to get her to love broccoli.
Ok, I lie.
When I was first diagnosed with cancer, it was a huge wake up call for me to evaluate my lifestyle and made me aware of how unhealthy I was living. Because I was so scared that cancer would get the best of me, I was hugely motivated and changed my eating habits instantly.
I would juice a few times a day, eat all the cruciferous vegetables, minimised my meat consumption and avoided dairy and sugar. It was easy peasy because at that point in my life, fear was driving me to eat healthy in a way I had never done before.
However, it’s now been six years from diagnosis. The anxiety and fear of a cancer recurrence has somewhat dissipated and frankly so has my motivation for healthy eating.
My life also looks different now. Busier. (Who's life isn't?).
I'm now focused on caring for my daughter. And it's hard work, taking up all my time and energy.
I've finally managed to get her to love broccoli.
Ok, I lie.
She's finally developed a taste for the green florets. The stem? Not so much.
She's only 18 months, so she hasn't gotten to the stage where she is super picky.
But what about when she gets older?
Healthy eating or lack thereof starts when we're young.
The dishes she grows up eating will most likely be her favourite foods in the future. Think about your favourite foods? Most likely these dishes were the ones your mum cooked for you.
So I wonder, how else am I shaping her beliefs towards eating and food?
We don't think about it much, but food has powerful emotional, social and cultural associations.
The foods that we eat can be driven by these influences, so I'm not surprised that eating habits are hard to change.
“If my health declines, the people that will suffer most are my family.
”
For me, everyday is a battle of priorities. Take care of my daughter or take care of me.
Often I put her priorities ahead of mine. But isn't that what moms do?
We want the best for our kids, but I have to gently remind myself that my health is a priority above anything else in my life.
If my health declines, the people that will suffer most are my family.
It's hard to find a healthy balance. But at least I must try.
I could eat healthy before, so I know I can do it again!
Unlike last time, I want this change to be permanent. If I'm going to make an impact on my longevity, then I need to be consistent. Not just for a month, 2 months, not even a year. I need to do this for the rest of my life.
This time I won't be driven by fear, but by love. Love for my body, health, and family. I'm a mother now, so I need to be an example for my little girl.
So to get started and get back on the right path, I wanted to gain some insights into other people's healthy lifestyle.
I asked nine amazing women bloggers in the health & wellness field, what their tips are for busy people who want to eat healthy and avoid the junk food and take-out.
Check out their responses below. I'm sure they'll be as helpful to you as they are to me.
Before you read their responses below, think about what's stopping you from eating healthy?
Which tip would be most helpful to you? Do you have any tips to share? I'd love to hear from you in the comments below.
Amanda Barnes (registered dietician @ Amanda barnes nutrition)
"Don’t leave junk food around the house. Having a bowl of candy or access to junk food often leads to mindless eating. Instead have a bowl of fruit or healthy snacks already prepared. If you are really craving sweets try to make them a bit healthier- dates, dark chocolate, or a chocolate avocado pudding. It will satisfy your sweet tooth without compromising too much on health. As for fast food, I like to have a few quick go-to meals so when I don’t have time to cook I am not left without options. Veggie burgers in the freezer, frozen vegetables and rice for a quick stir fry, if you know you have options you won’t have to go for the fast food."
Cassie spanner @
"Meal prep is key! You don’t have to go crazy like those people I see who prepare an entire week's worth of meals and snacks on a Sunday! Just start with making a bit more food for dinner so you have leftovers for lunch. Or planning your snacks for the week so you steer clear of your work’s biscuit jar. Also pick weeknight dinners that are easy to prepare (ready in less than 30 minutes) but also delicious so you aren’t tempted to stop on the way home and pick up some takeout. "
amy miller @ I heart the new me
"Meal prep is a tremendous help. Make a plan for the entire week. It also helps with portion control and mindless eating. I like to make energy balls for before my workout and I make a crustless veggie quiche in a pie pan and cut slices all week long for breakfast."
Chantal Drouin-Charters @ Mindful munching
"Prep is key. Even if you don’t want to go into big meal preps, having a few things done ahead of time will help you tremendously. Figure out what types of foods you like that are quick and can be eaten on the go. Oatmeal can be made at the office or hotel, nuts and seeds can go anywhere, a good/clean food bar in your purse or car for emergencies.Make a large cold bean salad to keep in the fridge and grab a serving when you’re short on time."
Wendy Hodge (precision nutrition certified coach @ Wendy's Way to Health)
"It all comes down to planning, but it doesn’t need to be complicated or time-consuming. Just find what works best for you. It might be planning a week of dinners, chopping up your fruit and veggies for the week or prepping your snacks. Always cooking more than you need when you do cook, is an easy way to have leftovers for lunches or to keep in the freezer. If you really have no time to cook, you can easily avoid take-aways by using a local healthy meal delivery service."
joanna zervas (accredited exercise physiologist @ balanced posture online)
"Meal Prep! If you want to make sustainable changes, you need to set aside time to buy healthy foods and prep your own meals on your free time. I like to make a huge Sunday and Wednesday dinners so I have leftovers for the other days or for the freezer. I also pack food items that I can keep in my bag or workstation, such as nuts, protein balls, or cans of tuna - which stink, but they’ll get me through a few meetings without a rumbling belly. I also source out surrounding areas for healthy food options, so if I need to get take-away, I already know where I’ll go and what menu items to order. "
Susan minich @ my real dish
Meal prep is so important. Spending an afternoon of chopping and cutting to make crockpot freezer meals saves me! It’s an easy way for me to have something that I thaw the night before and throw in the crockpot. I’ve had luck with Wildtree Organics (if you are in the US look into it!). They have organic healthy sauces and spices, and tasty easy freezer meals recipes. Also, on Sundays I prep my veggies and salads for lunch and overnight oats and smoothies for breakfast, so that I can quickly walk out the door in the morning. Meal prep makes my life less stressful and eliminates my need to eat out.
Mj ong
(accredited exercise scientist, pregnancy, postpartum health & fitness coach @ the baby wearing health coach)
Planning ahead helps tremendously. At our house, we usually do a big shop on one day and we will wash all the fruits and vegetables and cut it up, ready to eat. But as life happens to us and we do need to quick meal, there is still takeaway and fast food that are healthier than others.
Ciara Doran @ cool things i love
A way to avoid junk food is to steer past that aisle in the supermarket and keep them out of the house. Out of sight out of mind.
How I Handled Fear After My Cancer Diagnosis
When I was diagnosed with breast cancer at the age of 29, I feared for my life.
No one close to me had been affected by cancer so I thought getting diagnosed was a death sentence. Six years on, I know this is not true because I’m still alive and still NED, short for no evidence of disease.
But back then, when my doctor broke the news that the lump in my left breast was not benign but cancer, those first few nights terrorized me. I was petrified.
When I was diagnosed with breast cancer at the age of 29, I feared for my life.
No one close to me had been affected by cancer so I thought getting a diagnosis was a death sentence. Six years on, I know this is not true because I’m still alive and still NED, short for no evidence of disease.
But back then, when my doctor broke the news that the lump on my left breast wasn't a fibroademona but cancer, those first few nights terrorized me. I was petrified.
What was I to do? I was in massive shock.
I wished someone had told me the answer all those years ago.
Instead I had to work it out for myself.
So today I want to tell you how I overcame fear, so that you can concentrate on what's important, which is getting your health back.
So let's start from the beginning......
...... when I got the awful diagnosis of breast cancer.
It was a strange feeling because it was the first time I had faced the possibility of death. But sitting in the doctor's office, alone, and feeling numb, my body was fine and physically intact. So how can death be so close?
Unlike in a car accident where we can suffer from major physical trauma and the end is quick, when we've just been diagnosed with cancer there is no bleeding, nor are we in great physical pain. I knew death was looming but don't really know when the exact moment will be.
And I think that's where the cruelty of cancer lies. We are in a great deal of emotional pain, not knowing what the future holds for us.
Telling family would have to be the top worst moments of my life. It was like breaking their hearts into tiny little pieces and not knowing how to fix it.
When I was diagnosed I was super young, in my late 20s and had my whole life ahead of me. When you're that young you feel invincible. Who thinks about cancer at that age? It wasn't a blip in my radar until cancer was right there pressing down on my chest until I couldn't breathe.
What I feared most was dying and never achieving life's big goals and dreams. Never getting married, never starting a family , never holding a sweet newborn baby in my arms, and never growing old with my partner.
Six years on from diagnosis, did I beat cancer? Time tells me that I have.
Was I fearless? DEFINITELY NOT.
I was afraid then, and I'm still afraid now that cancer will come back.
I call the fear of recurrence as Post Cancer Stress Disorder (PCSD). And most women that have gone through breast cancer has it to some degree. Fortunately it decreases in intensity over time but unfortunately the fear stays with us for the rest of our lives.
Similar to war veterans that suffer from PTSD, hearing a loud bang will cause them to immediately drop to the floor.
With breast cancer survivors, every ache and pain....
..........We automatically think it could be a recurrence.
Any lingering fatigue from cancer treatment we feel......
..........We automatically think it could be symptoms that the cancer is creeping back.
So for those who are newly diagnosed, and those who are years out from their treatment, how should we handle fear?
Well.........
We often hear people talking about fear as something you should:
fight off,
conquer it, or
punch it in the face.
Be fearless and fight cancer! Like we've signed up for extreme sports.
But what if we looked at fear from an evolutionary perspective?
Then we can see what fear truly is.
A normal response to danger.
Receiving a diagnosis of cancer means coming face to face with our mortality. So being afraid and fearful of cancer is totally okay.
We need fear in order to survive.
Remember all those times that your instincts saved your life?
Don't dive into the black water.
Don't catch a ride with that stranger.
Be careful of that steep cliff face etc., etc., you get my point.
Yup, that was fear.
Unfortunately, fear and other manifestations of fear (take anxiety for instance) is also there in our everyday lives, even if we're not in any physical danger.
The stress response that fear triggers causes massive changes in our biochemistry, which we commonly know as the fight or flight response.
Back in the good old days when we were cavemen and threatened by a predator, we were faced with two choices - we could either:
1) Run away from the danger or
2) Stay where we are and fight the lion.
Regardless of which path we choose, the body’s response is always the same. The stress hormone, cortisol and adrenaline is released causing the heart to beat faster, blood vessels constrict to minimise any potential blood loss, fuel is mobilized from the muscles, our senses become heightened and the mind becomes sharp.
The reason our bodies respond in this particular way is to propel us into action. Biology doesn’t want our bodies to stand still, frozen like a statue. If we did, we will get eaten by the lion and perish.
Of course we are no longer cavemen and women and live quite safely without the threat of predators lurking at the front door. However, in modern society, the stress response is triggered by seemingly lame and non-dangerous situations.
That dead-line you're scrambling to meet.
An argument with the spouse
Late for an appointment
Overdue bills to pay
Insert your own stressful life here _______.
So then why do we still feel fear when we're perfectly safe from harm?
Take public speaking for example.
Why are most people afraid of public speaking when we obviously know that we're not going to die?
At the very basic core, I think fear is an emotion that pops up when we don't know what the future will hold - we don't know what the outcome will be.
And the only thing fear tells our mind to do is STOP.
Stop whatever it is we're doing......
......Stop. Stop. Stop.
So I think there's a disconnect between what our mind is telling us, which is to stop.
And what our biology is telling us, which is to keep moving - run or fight.
Often when people are paralysed by fear - this can manifest into all sorts of unwanted physiological effects - headache, nausea, and depression just to name a few. This also why I think so many of us have anxiety.
But we're getting a little off track here, so let's get back to the topic of this post.
How do we handle fear when we've recently been given a cancer diagnosis?
Our bodies DON'T want to stand still. Our bodies DON'T want to be a deer in the headlights.
But our mind says STOP. STOP. STOP.
So how do we keep moving?
Because we do need to keep moving.
We need to be making important medical decisions with a calm and rational mind. Because it's those decisions we make in the first few weeks that will affect the long-term outcome of our cancer treatments.
Ask any woman that's received a breast cancer diagnosis and she'll tell you those first few weeks are emotionally the toughest.
It's when you have to:
break the news to family and friends.
choose your cancer team,
understand the pathology reports,
make sure nothing is amiss from your diagnosis, and
it's also the time to create a treatment plan with your doctors.
So how do we not let fear affect us negatively in those critical few weeks?
After years of contemplating I think I've finally figured out why some people can move forward so easily while others are held back.
"We need to be one per cent more curious than we are afraid."
Think about it:
Curiosity makes us look around dark corners and uncover a hidden gem.
Curiosity makes us jump off an aeroplane and feel the exhilaration at plunging free fall.
Curiosity makes us hike a torturous climb to the top of a mountain just to feel the breeze at the peak.
Basically curiosity will allow you to move forward and propel you to do things in spite of not knowing how the ending will be, in spite of you being afraid. It's ok to be afraid.
We don't need to be fear-less, but we can be brave when fighting cancer.
So how did I come to this realization about curiosity?
How did I know it was my antidote to fear?
Well I traced back to my footsteps 6 years ago. These four things that I'll mention were the things that got me through those first few weeks and .........
...............it all boiled down to my curiosity.
It helped that my background is a researcher, always questioning the hypothesis (or the status quo). But you definitely don't need a degree to be curious!
1 | What Am I Afraid of? ........ Really.
Sometimes our emotions can be irrational. Fear likes to hide in the shadows of the unknown.
So get specific about what you’re afraid of.
Obviously you’re scared of death, but what part of that is frightening?
Are you afraid of what happens to you during treatment? or the dying process?
For me personally, I was so scared of leaving loved ones behind! But when I talked about it out loud, I realised that if I died, it wasn't the end of the world.
Everyone will eventually move on with their lives. It was SAD, yes.
But scary? ..........Not really.
Start getting deep with yourself and explore the root of these emotions.
Most importantly share those fears with people close to you, say them out loud and discuss possible scenarios if things take a turn for the worst.
How will that actually eventuate in real life? Perhaps it wasn’t as scary as previously imagined.
2| If Cancer Was a Puzzle, There Must Be a Solution.
I truly believe that we need to be our own advocate and make medical decisions together with our doctors. Our doctors are our educators, our medical partner and facilitator.
However, the reins are still mine and yours to take.
Just because a person wears a white coat and have a medical degree doesn't mean they are faultless. I have great respect for the medical profession, but most women including myself were given only one option for treatment.
From my experience there's always more than one way to do something.
You see, the doctor usually gives you the option that he thinks is BEST for you - which usually means making assumptions about you.
It's your job to figure out what these assumptions are and whether they are true or not.
Whilst alot of women will come in for a consult, distraught and expect to be told what to do, I gained more respect from the doctors when I was able to be calm and come in prepared for the consult.
My oncologist half jokingly said that he had to prepare himself before our consults, because I always asked the tough questions!
However, in order to effectively do this, it's important to not let fear paralyze our minds.
We need a lot of brainpower to solve this cancer puzzle. Otherwise, in the end, we will be left with odd pieces that don't mean anything.
We want to be our own advocate and not regret the medical decisions we've made along the way.
3| Why Can't I Be the Exception?
The internet can be a scary place when searching for information on your exact type of cancer. Words like “aggressive” and “fast growing” kept popping up in my searches. I even went further and looked at survival statistics on triple negative breast cancer patients. Let's just say the odds weren't in my favour.
One night as I was googling away in front of the computer, I managed to come across a breast cancer forum. Each person that logged in could write specific details about their cancer journey under their user profile. They had dates of diagnosis, details about their treatment such as the names of chemotherapy drugs and how many radiation treatments they had. It just so happened that a woman that was active in the forum was a triple negative breast cancer survivor for 15 years and to this day still NED!
So I asked myself, why not me?
Why can't I be the one that survive this?
Simply knowing there were long term survivors made me forget about the statistics. I realized that everywhere in nature, there were huge variations in everything! Even two people with the same subtype of cancer that received the same treatment can have vastly different outcomes.
This is because they have different genetics and more importantly they lived in two separate environments.
Technology isn't here yet to enable us to change our genetics.
But we can alter our lifestyle.
So I came to the realisation, there must be something that I'm doing to contribute to the cancer growing.
Despite my oncologist telling me that I've done nothing wrong, I honestly don't believe in bad luck. Bad luck just means we are helpless to help ourselves.
I really needed to know what those factors are that contributed to my cancer, and more importantly how to avoid them so as to avoid a recurrence later on! Which leads me to my last question.
4 | Was This a Wake Up Call To Take Care of Me?
This was the one question I was really excited about to find the answer. Looking back, even though I was in the medical field, I really had no idea what health looked like. Over the previous years my body had deteriorated so badly. I felt lethargic, my skin was covered in pimples, I had bad migraines and I was constantly sick with a cold.
Now that I was diagnosed with cancer, I had a great reason to ditch the bad lifestyle habits.
I truly believe cancer is a symptom when your body breaks down.
I never took care of myself, I was always stressed out. Cancer was my internal warning system telling me to wake up and start taking care of myself.
So before I started my treatments I raided the bookstore and stumbled upon a book called Anticancer A New Way of Life by Dr David-Servan Schreibber.
I questioned all my beliefs about food, exercise and how it contributed to health. I evaluated my whole lifestyle and started making changes.
Often women and in particular mothers are so good at taking care of others that they often neglect to take care of themselves. Remember those safety procedures in a flight emergency? It’s critical you put your own oxygen mask on before you help others.
Don’t you think it’s time to start putting yourself ahead of everyone else - because if not now then when?
So there you have it. The four things I was curious about that helped me move forward after a breast cancer diagnosis. I promise you that curiosity will be your new best friend, IF you'll let it guide you in your cancer journey. I will end this post with a quote from Albert Einstein.
"I have no special talent. I am only passionately curious"
Now I would like to hear from you in the comments section below. How did you react to your breast cancer diagnosis? Do you have an antidote to fear that you would like to share with us?
PS: If you like this post don't forget to share this article!
Trifina Sofian has a PhD in Biochemistry and is a cancer survivor, and mother. She was diagnosed with Stage 2b triple negative breast cancer in 2010 at the age of 29. Trifina is a Mindset and Life Coach. She helps others gain clarity & focus during cancer treatment and find their "new normal". Her mission is to help others move past their fears and limiting beliefs and gain back control of their life. She also has a blueberry smoothie every morning. Learn more..